
The newly elected Northern Territory government has committed to rolling out the massive Core Clinical Systems Renewal Program (CCSRP) despite its precarious budget situation, chipping in an extra $73 million to the original $186m price tag for the system, which will consolidate all of the NT’s public health clinical systems into a single ICT solution.
First announced last last May with a tender released in August, four shortlisted contenders are in the running for the five-year project with the successful tenderer expected to be announced in May. The shortlist includes local player Telstra Health, US EMR giants Epic and Allscripts, and fellow US company InterSystems, which markets the Australian-designed clinical system TrakCare.

The memorable phrase first coined by Adelaide GP Tori Wade that telehealth in Australia has “more pilots than Qantas” got a nice little workout at the Australian Telehealth Conference (ATC2017) in Melbourne this week, but while it may be in vogue for a little bit longer, the consensus seems to be that we are beginning to see the move from itty bitty pilot projects to embedding telehealth as business as usual in the provision of healthcare.
That may not necessarily be true as yet in primary care, predominantly due to the funding model, but it is certainly beginning to be seen in secondary care, particularly for outpatients services for rural patients and but also in emergency care in regional areas where specialists are hard to come by. All states and territories are now taking telehealth seriously, even the small ones, and a lot of the thanks for that is due to a mixture of political enthusiasm for sexy tech but also the hard yards that a number of clinical groups in a number of states have done over the years.

Standards Australia has set a revised date of June 30 for the publication of the Digital Hospital Handbook, belatedly issuing a statement saying the document was finalised but was under review by governments.
Standards Australia had originally planned to release the handbook last month, telling Pulse+IT in February that it would be published in March. However, a decision was then made to delay the publication, with the standards organisation refusing to explain why.

The driving forces behind the successful Victorian Stroke Telemedicine (VST) program are hoping to set up a national telestroke network to ensure people living in regional areas can avoid the “postcode bingo” that often sees them receiving a lower level of stroke care than people living close to metro hospitals.
The pioneering program has just gone live at Wonthaggi, its 16th and final hospital in regional Victoria, allowing emergency department clinicians throughout the state to have 24/7 access to a consultant neurologist who can diagnose a stroke from a distance and immediately order treatment or transfer.
VST clinical program lead Chris Bladin told the Australian Telehealth Conference in Melbourne today that since the program first commenced in 2012-2013 with $7.3 million in funding from the federal Health and Hospitals Fund, almost 1500 consultations have taken place and many patients have been transferred to Melbourne for endovascular clot retrieval or treated with clot-busting thrombolysis, with sometimes remarkable outcomes.

How many times have you called an organisation only to be greeted by an integrated voice response system? Your frustration builds as you struggle with your phone to choose the right option.
Over the years, smarter organisations have introduced voice recognition services and innovative smartphone platforms, like Nuance, Interactive Intelligence and DialMyApp. Working together, these solutions can verify your voiceprint and use the capabilities of your smart phone to bypass the IVR.

An integrated care service based at Launceston General Hospital has gone live with a new referral management system developed by listed Adelaide firm Alcidion to better automate the referral process, with the next step to work on electronic receipt of referrals from GPs and specialists and the ability to send messages back to the referrer.
The Northern Integrated Care Service (NICS) was first established in 2012 to provide accessible, integrated services for people with or at risk of developing chronic and complex health conditions. Service providers include the state-run Tasmanian Health Service, the state's PHN, known as Primary Health Tasmania, and the University of Tasmania.

Mobile workflow solutions specialist Ascom is set to begin shipping version two of its Myco healthcare-specific mobile device in June, adding new Google app functionality, near-field communication and infra-red location capabilities to the Android device, which also functions as a barcode scanner.
Myco is predominantly aimed at improving nurse workflow and has been designed as an all-in-one communications device, replacing multiple smartphones, pagers and and scanners. It can integrate with a number of hospital information systems, including nurse call, EMRs, real-time location services, patient monitoring systems and infusion pumps.

A sub-contractor for medical transcription provider Global Transcription Services (GTS) has been identified as the source of a recent privacy breach, in which letters from specialists to referring GPs concerning hundreds of patients were discovered in a rubbish bin in Sydney.
NSW Health has revealed that the incident mainly involved letters and progress reports about patients attending a number of public and private outpatient clinics last December, with 768 public patients involved and just over 700 pieces of correspondence relating to private patients.

The Australian Digital Health Agency (ADHA) has partnered with eHealth NSW and the Sydney Children’s Hospitals Network to set up a child health informatics network, concentrating on identifying digital technologies that can benefit children's health and their experiences of the health system.
Dubbed the Collaborative Network for Child Health Informatics, the initiative is being funded by ADHA and aims to bring together experts in children's health to identify national projects that will positively affect health and social outcomes for kids.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending April 23:
AMA, Regenstrief launch EHR training platform for medical students
Healthcare IT News ~ Mike Milliard ~ 19/04/2017
The American Medical Association on Wednesday announced a partnership with the Regenstrief Institute and Indiana University School of Medicine to launch an electronic health record training program for medical students.
Cybersecurity start-up exposed hospital network data in demos
Healthcare Info Security ~ Jeremy Kirk ~ 20/04/2017
Billion-dollar cybersecurity startup Tanium has acknowledged failing to thoroughly anonymize network information for a California hospital that appeared in live product demonstrations and online videos.

Besides a ramble from a slightly unhinged Pulse+IT journalist last week, which turned out to be our most-read article, the big news this week was the sale of specialist software vendor Genie Solutions to a proudly ethical private equity firm. The value of the deal is confidential but we understand it is substantial and so it should be.
Founder Paul Carr and his extended family deserve all the financial benefits that come from having done the hard yards to build Genie into a popular product and a substantial Australian health IT company over the last 22 years.
The IPN Medical Centres group has officially announced it will roll out Precedence Health Care's MediTracker app to its 180 practices, allowing two million patients to have access to a summary of their data held on their regular GP's medical record.
MediTracker has been trialled in select IPN practices since the start of the year, with GPs contributing to the app’s design and functionality. Any practice using the MedicalDirector, Best Practice or Zedmed clinical information systems can also offer it to patients.

Standards Australia is staying silent on the reasons behind a delay in the publication of the promised 'world-first' Digital Hospital Handbook, citing a lack of resources as to why it has not made an official announcement and also refusing to put a timeline on when the publication will finally be ready.
Standards Australia CEO Bronwyn Evans told Pulse+IT in late February that the handbook, which was provided with $100,000 in seed money by the Victorian Department of Health and Human Services (DHHS), would be available the following month, but less than three weeks later informed a conference in Sydney that it would miss its deadline.

EMR giant Allscripts will offer its dbMotion interoperability platform to the Australian and New Zealand healthcare markets as a cloud solution via Microsoft Azure, promising faster implementation and lower upgrade costs than the on-premise version.
dbMotion, which Allscripts bought in 2013, is a service-oriented architecture solution that allows disparate pieces of health data held in different systems and sites to be brought together as a de facto patient record at the point of care.

Superannuation fund-backed private equity firm IFM Investors has acquired a majority stake in market-leading specialist software vendor Genie Solutions, in a deal thought to be worth over $50 million.
Founded in 1995 by Paul Carr, who led the development of the company until handing over as CEO in November 2015, Genie is the market-leading vendor of clinical, billing and practice management software for medical specialists, with over 3500 sites in Australia.

The federal government will introduce a new Medicare rebate for people living in rural and remote areas that will allow the bulk of the psychological sessions subsidised under the Better Access program to be conducted by telehealth.
Set to cost $9 million over four years, the initiative will begin on November 1 and will be available for patients living in Modified Monash Model regions four to seven, which cover smaller country towns and remote and very remote locations.

It was an American radiologist called Adam E Flanders who pointed out the obvious truth in 2008 that “vendors do not deliberately design bad software”, but there is no doubt that there is increasing dissatisfaction being voiced by clinicians, particularly doctors in the US, about the clinical information systems they are asked to use.
Those criticisms are being heard closer to home as well, particularly about the electronic medical records that are fast being implemented in most healthcare settings in Australia.

The Torres and Cape Hospital and Health Service is set to launch a new dental health project in the Torres Strait as part of a $1.46 million grant for the region from the Queensland government's $35 million Integrated Care Innovation Fund (ICIF).
Torres and Cape HHS is working with the Northern Queensland Primary Health Network (PHN) on the primary oral health care project, which will see the introduction of intra-oral cameras and the use of existing video consulting technology to allow primary health workers to consult with dental staff at the main clinic on Thursday Island.

Orion Health has signed off on a much-anticipated deal with the Dorset County Council in the UK for a $NZ9.34 million electronic health record, and has also named a former executive with EMR giant Epic to run its global sales and marketing strategy.
The ASX and NZX-listed software vendor, which has seen its share price take a hammering over the last few months, has signed a five-year agreement with the county, which will see it roll out a comprehensive care solution based on its Amadeus precision medicine platform.

Telstra Health has set up a new advisory panel to provide operational and strategic advice to the business, snaring former RACGP president and Flinders University professor of global primary care Michael Kidd and former Mincom CEO Richard Mathews.
Telstra Health said in a statement that the panel will help support the execution of its strategy to integrate key health software, analytics and platform capabilities that it has acquired or partnered with to offer innovative services to the healthcare sector in Australia.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending April 16:
Hospital cuts costly falls by 39% due to predictive analytics
Healthcare IT News ~ Bill Siwicki ~ 12/04/2017
El Camino Hospital linked EHR, bed alarm and nurse call light data to analytics to identify patients at high risk of falls.
Alarm fatigue: 5 reasons nurses may have a delayed response to alarms
FierceHealthcare ~ Ilene MacDonald ~ 12/04/2017
Nurses typically respond quickly when alarms are urgent and life-threatening. But a new study finds they are slower to respond to them at the end of a long shift when they suffer from chronic alarm fatigue.

The Pharmacy Guild is working with the Department of Human Services to allow automated recording of immunisations to the Australian Immunisation Register (AIR) before next year's flu season.
Approved pharmacists in most states and territories can now administer the influenza vaccine to people over 18 and in a few jurisdictions the pertussis and the measles vaccine.

It's never nice to kick someone on the redundancy line when they are down but the sub-editor at the Daily Telegraph who decided to come up with a headline screaming about your optometrist finding out about all of your abortions because of the My Health Record seriously needs to reevaluate their career choices.
While we had a nice little story about pathology reports finally going up to the MyHR from public hospitals in NSW, over at the Terror it was full-on nonsense mode, in which the fact that access controls are set on universal by default is somehow a 'bungle'. It's not, they've always been like that, consumers can change them whenever they like and no, it doesn't mean 600,000 people will be exposed to your haemorrhoids.
A clinical performance benchmarking platform developed by Queensland start-up Osler Technology that allows hospitals to measure the clinical competencies of staff is being rolled out at Noosa Hospital on the Sunshine Coast, with Mackay Hospital also implementing the system to support the procedural elements of the junior doctor curriculum.
Osler Technologies has also rolled out its individual clinical passport app, which allows doctors and nurses to build a digital portfolio of their skills as they acquire procedural certifications, which company co-founder Todd Fraser said was also applicable to primary care clinicians, especially rural practitioners.

People with bipolar disorder are very positive about using mobile apps to help them self-manage their condition despite concerns about the quality of some apps in what is still an unregulated market, new research has found.
In an analysis published in the Journal of Medical Internet Research, Black Dog Institute researcher Jennifer Nicholas and colleagues, including well-known eHealth expert Helen Christensen, analysed 48 apps for bipolar disorder available on Google Play and the App Store.

Newly rebranded IT services giant DXC Technology is focusing on the growing movement towards integrated care as it seeks to replicate the success of its Lorenzo digital platform in the UK in the local market, promising to go 'beyond the walls of the hospital' to link up acute and primary care.
DXC – which came into being following the merger between CSC and the Enterprise Services division of Hewlett Packard Enterprise last week – has been working on localising Lorenzo in three different areas: national infrastructure requirements, billing and legislative reporting.

Adelaide-based Clintel Systems has launched a tailored solution for plastic surgeons and cosmetic day surgeries called CareRight PS.
CareRight PS is a web or server-based software solution that builds on the existing capability of Clintel’s CareRight solution for specialists and day surgeries, with added functionality required by the plastic surgery discipline.

The New Zealand Ministry of Health is gearing up for its much anticipated tender for a strategic IT solution for the National Bowel Screening Program.
The $NZ40 million program is due to kick off at the Hutt Valley and Wairarap DHBs in July, with extra money put aside for the IT required for a national program. Bowel screening will be offered to eligible people aged 60 to 74 every two years.

NSW has begun sending pathology reports from public laboratories in south-eastern Sydney, the Illawarra and the Children's Hospital at Randwick to the My Health Record, with western Sydney and western NSW to begin next month, followed by the Northern Territory.
NSW has already uploaded 4170 reports to the MyHR through its HealtheNet clinical data repository, which allows data to be shared locally and with the national system. In line with an agreement between the Commonwealth, the jurisdictions, the college of pathologists, NEHTA and the wider industry in 2014, the full pathologist's report is being uploaded as a PDF in a clinical document architecture (CDA)-compliant wrapper.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending April 9:
Patients to get access to GP records via NHS.uk in September 2017
Digital Health News ~ Laura Stevens ~ 06/04/2017
Patients will be able to access their GP record via the revamped NHS.uk from September 2017, according to NHS Digital.
Citizen Identity project will be live by October 2017
Digital Health News ~ Laura Stevens ~ 04/04/2017
The papers say the project is “providing a single, secure identity for each member of the public, across all health and care services”.

Poor old Orion Health took an absolute bath on the stock exchange this week, its share price plummeting 15 per cent on Monday and another 14 per cent on Tuesday after it provided an update to the market. The reason? A slightly lower revenue forecast, a shrinking bank balance and a few new contracts sliding into FY 2018, including a small but important win to provide a shared care record in the county of Dorset in the UK.
Orion is doing well in the massive US sector, which has been its largest market for some time, but it's likely that the company will have to ask investors for a bit more dough in the short term or start to draw down on its debt facility. As a health IT company like Orion is a long-term bet, you do have to wonder what the scaredy cats who deserted it this week were doing investing in the first place.

HL7 Australia is working on a localised version of the FHIR specification as local implementations start to take off, with early adopter Telstra Health already exploring its potential to link up its disparate business units, implementations in several medications management projects and a mobile gateway for the My Health Record under development.
FHIR creator and product director Grahame Grieve said national implementation guides were likely in each country, much like the recent core implementation guide for the US, which was issued at the same time as the third edition of the draft standard for trial use (DSTU) last month.

ACT Minister for Health Meegan Fitzharris has released the terms of reference for the promised system-wide review into ACT Health's data management and reporting problems, which saw the department fail to make deadlines for reporting performance figures to the Productivity Commission and the Australian Institute of Health and Welfare.
The missing AIHW data also meant that figures on the Canberra Hospital was left out of the AMA's annual national public hospital report card, released in February.

A new Centre for Virtual Health Innovation that aims to use technology to support patients to manage their own health and access expert advice no matter their location or circumstances is the first initiative launched under a new joint venture between Waikato District Health Board and the the University of Waikato.
The two organisations, which are also bidding to build a third medical school in New Zealand – to the consternation of the two traditional medical education providers, the universities of Auckland and Otago, which have countered with a bid to build a GP-focused School of Rural Health – have officially launched the Waikato Institute of Medicine and Health, which will focus on promoting and providing innovation in health and medical education, health technology and health service delivery models.

Registrations have opened for the Health Informatics New Zealand (HiNZ) conference, being held in November in Rotorua.
Featuring a presentation from the NZ Ministry of Health's chief technology and digital services officer Ann-Marie Cavanagh, places are still open for people interested in presenting a scientific paper, digital health idea or clinical case study.

Melbourne's Western Health has signed a five-year, $2.35 million contact with Adelaide health informatics firm Alcidion for its Miya platform, including applications for results, ED, and patient flow and bed management, accessible on iPads and other mobile devices in wards and clinical areas.
Alcidion has a long-standing relationship with Western Health, which encompasses the 600-bed Sunshine Hospital, 290-bed Footscray Hospital, the 90-bed Williamstown Hospital and the Sunbury day facility.

Fitness bands may well have been among the first widespread consumer-driven instance of personal health monitoring, but advances in technology have since changed healthcare forever.
Clinics, hospitals and healthcare providers throughout Australia are adopting clinical and practice management solutions that reflect advances in technology and related legislation and standards that ensure data privacy and security.

General practitioners in NZ's Northern region now have single sign-on access to the TestSafe clinical data repository through the My Practice and Medtech32 practice management systems, allowing them to log on once per session and see their patients' results with the click of a button.
TestSafe is a shared clinical information service first established at Auckland's Middlemore Hospital to allow hospital doctors to see lab results. Based on Sysmex's Eclair clinical data repository (CDR), it is now used by all four Northern region district health boards and and has since grown to contain diagnostic results and reports, clinical letters, discharge summaries, copies of eReferrals and data on medicines dispensed by community pharmacists.

The Health Information Management Association of Australia (HIMAA) has issued a call for abstracts for the national conference it holds in association with the National Centre for Classification in Health (NCCH), taking place in Cairns in November.
The theme of the fourth annual HIMAA NCCH national conference is 'Challenging a Changing Landscape', which HIMAA says reflects the ground-changing influence health information professionals are having on the landscape in which they work.

SA Health has signalled its intention to begin the full roll-out of its Enterprise Patient Administration System (EPAS) at Flinders Medical Centre and the new Royal Adelaide Hospital, issuing a tender for a fleet of workstations on wheels (WOWs), which are required to support the EPAS application suite of laptops.
EPAS, which has come in for more criticism recently, this time from a South Australian coroner, has been deployed at FMC in a read-only version for some time. At the new Royal Adelaide, where staff training has begun before an expected opening later in the year, the patient administration module will be implemented first before the full clinical suite goes live at a later date.

Auckland-based health IT firm Orion Health is still aiming to be profitable in the 2018 financial year and has recommitted to its R&D program despite forecasting lower than expected operating revenue for the current year, which saw its share price slump by 14.5 per cent.
Orion Health, which listed on both the New Zealand and Australian stock exchanges in late 2014 at an initial price of $NZ5.70, is trading at about $1.42 today. It had been trading steadily last year at about $3.50.

The Australian e-Health Research Centre (AEHRC) has received renewed funding for another five years, with joint venture partners the CSIRO and the Queensland government chipping in $25 million to keep the national research body operating.
The AEHRC, which is headquartered at the Royal Brisbane and Women's Hospital but has offices in Perth, Sydney and Melbourne, was first established in 2003 to develop ICT innovations in healthcare. It also has a partnership with WA Health with an emphasis on telemedicine and ocular imaging technologies.

At almost every health summit or forum, Australia's lack of systems interoperability is a big topic. The consensus is that, as a system, the health sector struggles to identify chronically ill patients and deal with their conditions effectively.
A partnership in Western Australia is solving such problems using an interoperable shared record system developed in a collaboration between the Silver Chain Group, WA Country Health Service (WACHS) and Queensland company Extensia to link other community records. When required, it can also upload them to the national My Health Record system.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending April 2:
Four more acute global digital exemplars confirmed by NHS England
Digital Health News ~ Laura Stevens ~ 31/03/2017
The additional four acute global digital exemplar trusts have finally been confirmed by NHS England, after being revealed in trusts’ board papers previously.
S Health relaunches as Samsung Health, adds telemedicine integration and more
MobiHealthNews ~ Jonah Comstock ~ 30/03/2017
As it launched its Galaxy S8 and S8+ phones, Samsung also quietly announced the re-invention of its S Health app as "Samsung Health".

Queensland's new 10-year digital health strategy, a sneak peek at the new Monash Children's Hospital, the establishment of a diagnostic imaging program and a strong opinion piece by HIMAA CEO Richard Lawrance on the shaky state of the health information management professions were all popular stories this week, but one that caught our attention concerned a topic we have been following closely for some years now: real-time monitoring of prescription drugs.
While the Pharmacy Guild's MedsASSIST system was set up as part of a multi-pronged strategy to resist the rescheduling of pharmacy-only (S3) medicines containing codeine to prescription-only (S4), the development of the system showed what could be done if there was a will and a way. As everyone in the healthcare industry knows, the Guild is a force to be reckoned with and the power of its lobbying strength puts almost any other industry association to shame, and while it ultimately lost the battle to keep sales of codeine-containing analgesics over the counter, the speed with which it designed, built and rolled out MedsASSIST showed what it can do when it sets its mind to it.

Queensland GP and Australian Digital Health Agency (ADHA) board member Eleanor Chew will discuss the pilots being planned for the Health Care Homes initiative, the funding changes being explored and the new opportunities the initiative presents for telehealth and digital access to the home at the Australian Telehealth Conference being held in Melbourne next month.
Dr Chew was a member of the Primary Health Care Advisory Group (PHCAG) that supported the introduction of Health Care Homes to reduce fragmentation of care for chronic disease patients and introduce new funding models for primary care.

On Wednesday, 22 March, NSW Health held an eHealth NSW Chief Clinical Information Officer's Clinical Engagement Forum entitled 'How do we put nurses and midwives in the driver’s seat for future changes to the eMR?'
Not a single health information management (HIM) professional was on the session’s panel of experts, even though HIMs are widely recognised within NSW Local Health Districts as the real drivers of EMR implementation.

The Pharmacy Guild has held off on plans to shut down the MedsASSIST real-time monitoring system for over-the-counter analgesics containing codeine, saying it had received support from Health Minister Greg Hunt to keep the system running until further advised.
The Guild announced yesterday that it planned to pull the plug on MedsASSIST tonight after a final decision by the Therapeutic Goods Administration and the Department of Health to up-schedule OTC codeine-containing products, such as painkillers and cold and flu remedies.

The Pharmacy Guild will close down the MedsASSIST real-time recording system it developed for monitoring over-the-counter codeine sales from tomorrow, saying the up-scheduling of codeine-containing analgesics to prescription-only rendered it obsolete.
The Guild first rolled out MedsASSIST last year in an attempt to ward off moves to up-schedule OTC codeine products, building and deploying the system through GuildLink and achieving take-up rates of 70 per cent.

Entries have opened for the annual Clinicians' Challenge, a joint initiative between the NZ Ministry of Health and Health Informatics New Zealand.
Health Minister Jonathan Coleman said a key focus of this year’s challenge is ‘disruptive innovation’, in which an innovation disrupts the existing norm and becomes the new benchmark.
Gosford Private Hospital, the Mater Hospital in Brisbane and the Mater Private are three of the expected five hospitals that are involved in a CSIRO-led trial of a smartphone app that delivers pre-surgery preparation and post-surgery rehabilitation for patients undergoing total knee replacements.
The trial, which kicked off last November and aims to recruit 300 patients to test the technology before launching it on the market, is being led by researchers from CSIRO's Australian e-Health Research Centre, Health and Biosecurity and Data61.

The Victorian government has named the 15 successful projects that will share in $5 million in extra funding for telehealth links to metropolitan specialists for patients living in regional and rural parts of the state.
The Victorian Telehealth Specialist Clinic initiative funding was first announced last year as part of the Department of Health and Human Services's (DHHS) strategic review of telehealth. which also looked at how to enable health services to access Healthdirect Australia's WebRTC-based telehealth solution VideoCall.

Queensland Health has released a long-term strategy laying out its vision for digital health in the Sunshine State, identifying eight system-wide strategic goals for advancing healthcare through digital innovation.
Designed to accompany 2015's landmark $1.26 billion eHealth Investment Strategy and the government's My health, Queensland’s future: Advancing health 2026 plan released last year, the Digital Health Strategic Vision for Queensland 2026 will be reviewed annually through a 'digital health check' to monitor progress.

The ACT government has come up with over a million dollars to pay for outsourced clinical coding services as a supplement to its in-house coding team at Canberra Hospital as workforce shortages continue to hinder its attempts to provide mandatory data in a timely manner.
ACT Health has issued a tender for two years' worth of remote clinical coding services with an option for a 12-month extension at $400,000 per annum, with the contract due to start on July 1.

Victorian Premier Daniel Andrews and Health Minister Jill Hennessy have presided over the official opening of the brand new, $250 million Monash Children's Hospital at Clayton, which will have a community open day this Sunday before patients begin moving in on April 19.
Serving south-east Melbourne, the Mornington Peninsula and Gippsland, the new 230-bed hospital includes 96 paediatric beds, 12 cancer day beds, 20 same day beds, 10 paediatric intensive care beds and 30 neonatal intensive care cots.

The Northern Territory government has asked that the company building the National Broadband Network (NBN) swap plans to provide the NBN to dozens of remote communities via satellite for a fixed wireless solution using existing fibre technology, saying the Sky Muster satellite is not reliable enough to provide necessary health, education and business services.
In a submission to an inquiry being held by the Commonwealth's Joint Standing Committee on the NBN, the NT said the “technically inferior” satellite service and its idiosyncratic nature would make it “difficult, costly or impossible” to ensure delivery of some online applications, and this had particular ramifications for health.
The diagnostic imaging (DI) sector is set to pick up where it left off in 2014 on work to get radiology reports uploaded to the My Health Record system and available to consumers and healthcare providers, with a longer term aim of developing the interoperable digital infrastructure needed to enable access to the images as well.
Earlier this month, the Australian Digital Health Agency (ADHA) convened a new diagnostic imaging program steering committee co-chaired by the Royal Australian and New Zealand College of Radiologists' (RANZCR) informatics representative Nick Ferris, who also worked on the National E-Health Transition Authority (NEHTA) group that completed a specification in 2014 for uploading radiology reports in PDF format.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending March 26:
A 40-year 'conspiracy' at the VA
Politico ~ Arthur Allen ~ 19/03/2017
The Department of Veterans Affairs built perhaps the most important medical computer system in history. Now it’s about to spend billions to throw it away.
GE to invest $500 million in healthcare and hire 5,000 software developers
Healthcare IT News ~ Bernie Monegain ~ 23/03/2017
GE will invest $500 million in its healthcare unit to make its operations more digital, and GE Healthcare also plans to double its bench of 5,000 software engineers, GE Healthcare CEO John Flannery revealed.

In news that will come as a surprise to no one, the state and territory health ministers, along with new federal Health Minister Greg Hunt and special guest NZ Health Minister Jonathan Coleman, met in Melbourne today for one of their regular COAG Health Council hoedowns and agreed to adopt the opt-out participation model for the My Health Record on a national scale.
Exactly when the move will be triggered is anyone's guess as the exercise will probably cost squillions, but there has long been a consensus among the powers that be that a critical mass must be reached if the thing is ever to be of use and it was always more than probable that opt-out would be given the go-ahead. Dr Coleman would have taken an interest in today's developments as they are planning a national EHR across the ditch as well.

HL7 International has published release three of the Fast Healthcare Interoperability Resources (FHIR) standard for trial use (STU), containing thousands of changes in response to the experiences of what are now hundreds of implementations around the world.
FHIR, the brainchild of Melbourne-based health informatician and standards guru Grahame Grieve, is a highly flexible and modern specification framework that uses contemporary web standards and an API based on modern internet conventions.

IT services giant CSC is gearing up for the finalisation of its merger with the Enterprise Services division of fellow global player Hewlett Packard Enterprise (HPE), with the combined company – worth $26 billion in annual revenue – to be known as DXC Technology.
The new company will be a big player in health IT in Australia and New Zealand, combining well-known brands owned by CSC such as iPM, webPAS, MedChart and iPharmacy, new offerings such as the Lorenzo digital platform, the Microsoft, Oracle and SAP capabilities that CSC acquired with the purchase of UXC in 2016, and now the broader customer base and complementary services from HPE Enterprise Services.

An independent evaluation of the Health Care Home (HCH) model established in New Zealand in 2011 has shown there are measurable positive benefits to patient experience, clinician satisfaction and delivery of care, although it is not yet showing any significant effect on levels of hospital admissions.
The evaluation was carried out by Ernst & Young (EY) on behalf of the so-called N4 Primary Health Organisations (PHOs) – ProCare, Compass Health, Pegasus and Pinnacle Midlands Health Network (PMHN) – with the latter having first customised the model for the NZ setting and implemented it in 15 practices in its region.
Adapted from the model developed by Group Health in Washington state in the US and set to be trialled in Australia, Health Care Homes are modelled around a team-based approach with the patient at the centre of care. The model uses a mixture of current and emerging technologies, including alternatives to face-to-face care such as telephone and email.

Best Practice Software (Bp) has closed registrations for its annual summit on the Gold Coast next month as the event has been oversubscribed.
Bp chief relationship officer Lorraine Pyefinch said the summit is always designed to be an intimate event with hands-on sessions and networking, and as such the 300-odd attendees currently registered is the limit.

Deakin University researchers developing a non-invasive smartphone-based solution for blood glucose monitoring will now proceed into the visualisation and prototyping phase with the assistance of the user experience design experts from Melbourne firm Navy Design as the inaugural recipients of Navy's Design Aid program.
The program aims to help underfunded digital health projects with access to healthcare-specific UX design expertise and will be offered by Navy Design twice a year.

Sydney-based ACSS Health has launched a configurable pre-admissions forms system aimed at day hospitals called Preadmit, which can integrate with the company's SimDay patient administration system or act as a standalone system for those using other brands.
ACSS Health, which also markets the well-known eClaims medical billing system, has been working on Preadmit for some years but has seen an increase in demand from customers predominantly over the last two years, operations manager Michelle Romero said.

An environment of cautious optimism seems to have descended on the players at the pointy end of the long-running saga of secure messaging interoperability – or lack thereof – with healthcare providers, software vendors, primary health networks and regulators now all working collaboratively on the issue.
There are still a number of challenges to be faced and the industry is only in the early stages of the proof of concept trials that the Australian Digital Health Agency (ADHA) put out for expressions of interest (EOI) back in January, but the consensus of opinion seems to be that an interoperable system will happen, despite the fits and starts that have plagued the technology's development in Australia over the last five or six years.
For Tom Bowden, CEO of messaging vendor HealthLink and vice president of the Medical Software Industry Association, there are still some hurdles to overcome.

Queensland Health has put out an offer for a service provider with design, build, test, operate and migration capabilities to help with its statewide enterprise integration platform replacement project, which will see the existing JCAPS-based middleware system replaced with Orion Health's Rhapsody integration engine for clinical systems.
Orion Health won the tender to replace the current mixture of Oracle's eGATE, JCAPS and Glassfish in late 2015. The project is essential to the eventual replacement of the HBCIS patient administration system but more immediately to the new laboratory information system, the winning vendor for which is expected to be announced shortly.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending March 19:
3 ways Trump’s FDA nominee could reshape digital health
FierceHealthcare ~ Evan Sweeney ~ 16/03/2017
President Donald Trump’s nominee to lead the Food and Drug Administration is a strong proponent of deregulating the drug industry, an approach that could be equally beneficial for the digital health industry that has occasionally butted heads with the federal agency.
Trump ‘America First’ budget plan calls for $15.1B cut to HHS
Health Data Management ~ Greg Slabodkin ~ 16/03/2017
The Department of Health and Human Services would suffer a $15.1 billion reduction in its Fiscal Year 2018 budget, and the National Institutes of Health would see its budget cut by $5.8 billion, according to a just-released plan from the Trump Administration.

By far our most popular story for the week was the announcement that Melbourne's Royal Children's Hospital had attained Stage 6 in the electronic medical record adoption model (EMRAM) framework developed by the US-based HIMSS, not just for its inpatient systems but for outpatients too.
While a framed certificate is all well and good if you get to hang it on your wall and it's even better if you've got two of them, the obvious question is whether an EMR is worth all of the time, effort and money put in. The total for RCH for that time and effort came to $48 million, which does make your eyes water a bit but which is pretty much par for the course these days when you take a mainly paper-based hospital to a fully digital one virtually overnight.

Roger Cook has been named as WA's Health Minister and deputy premier in Mark McGowan's newly elected Labor government and has had mental health added back to his portfolio responsibilities.
Mr Cook has acted in the role of shadow minister for health since his election to state parliament in 2008 and proved a dogged pursuer of former health minister Kim Hames over the Liberal government's perceived failings in health, particularly the commissioning and opening of Fiona Stanley Hospital and its IT woes.

The $2 billion new Royal Adelaide Hospital has reached technical completion after several delays, and will now enter a minimum 90-day testing and training period to ensure the landmark hospital is ready for patients.
South Australian Health Minister Jack Snelling announced yesterday that the hospital will begin to be stocked from today, with nearly 2000 pallets of equipment, technology and supplies arriving to be installed by logistics staff in the 800-bed facility.

Gold Coast Health has been able to eliminate patient queues at Gold Coast University Hospital's (QCUH) five busiest departments and reduce its did not attend rate after deploying the Q-Flow technology from customer experience software company NEXA.
Billed as a “patient optimisation framework”, the technology platform integrates with GCUH's core systems and captures critical performance data from busy departments such as women's outpatients, adult outpatients and children's outpatients as well as pathology collections and the hospital's cancer and blood disorders outpatient and day unit service.

Last year, Queensland-based firm Longevum started working with private home care provider Envigor to use its Gevity technology as Envigor's new health management platform for home monitoring.
This year, the company plans to add gamification capabilities to Gevity to supplement its offering to two other core markets: corporate health planners and insurers, who are increasingly investing in technological options to ensure their clients are well and stay well into the future.

Melbourne's Royal Children's Hospital has become the first in the country to achieve Stage 6 on the HIMSS electronic medical record adoption model (EMRAM) for both its inpatient and outpatient services, 10 months after going live with a $48 million implementation using an EMR from Epic.
It is also the first public hospital to attain Stage 6 EMRAM, joining the private not-for-profit St Stephen's Hospital in Hervey Bay, and the first to attain Stage 6 on the outpatient electronic medical record adoption model (O-EMRAM).
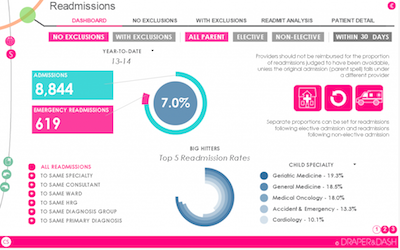
Global IT services and solutions giant CSC has agreed to act as a reseller for the UK healthcare analytics and data visualisation firm Draper & Dash in the Australian and New Zealand markets, promising that the combined offering will reduce implementation timeframes from years to weeks.
Draper & Dash offers a range of dashboard applications built on the QlikView platform that are customisable to hospital and health service data environments and information needs.

The Aduro interface that powers HealthLink's SmartForms technology has now been rolled out to 78 per cent of Australian general practices in what is a major step towards the implementation of a safe and secure eReferral capability similar to that used in the company's native New Zealand.
Aduro is a standards-based interface that enables a GP or specialist’s practice management system to communicate with a centrally hosted forms server and is the technology that underpins the mandatory electronic referrals system used by the three district health boards in Auckland, which is also being trialled here as part of the Victorian eReferrals Program.

Three in four Australians think it would be very or somewhat convenient if their eHealth records were available at their local pharmacy immediately after a doctor’s appointment to avoid having to repeat themselves, new research shows.
The Healthy Futures Report, commissioned by the Pharmacy Guild and conducted by McCrindle Research, also found that technology supports such as the ability to fill scripts requested by phone, email or SMS, receive notifications by app or SMS or receiving informative emails would help people take their prescribed medications.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending March 12:
Salford Royal will upload wearables data to personalise treatment
Digital Health News ~ Ben Heather ~ 09/03/2017
One of England’s most digitally advanced trusts will start uploading patient generated wearable data to its electronic patient record.
IDC: Hospitals undertaking digital transformation to skyrocket in 2017
Healthcare IT News ~ Jack McCarthy ~ 09/03/2017
While only 10 percent of healthcare providers and payers are currently working to digitize themselves, the analyst house estimates a big surge in the months ahead.

There was huge interest in our story this week on the MediTracker app that is shortly to be launched by Precedence Health Care, which will do what has so far been impossible in Australia and let patients see a summary of their GP medical record on their phone or iPad.
Along with the Healthi app made available a couple of weeks ago by Chamonix that gives patients mobile access to their My Health Record, the MediTracker app looks to be a bit of a game-changer for mobile access to health information in this country.

Canterbury District Health Board has gone live with the first implementation of the South Island's new patient administration system in an inpatient ward at Burwood Hospital, and has also finalised the full roll-out of CSC's MedChart electronic prescribing and administration system on the Christchurch campus.
The South Island Patient Information Care System (SI PICS) is being piloted in Canterbury at the new Burwood Hospital, which runs Canterbury's older person's health specialist services, including inpatient assessment, treatment and rehabilitation, community services and older person's mental health.

The Southern District Health Board has launched a new cardiology telemedicine clinic to provide remote cardiac services to patients at Dunstan Hospital in Central Otago.
Specially trained nurses will take measurements and support the patient at Dunstan while they talk to a cardiologist at Dunedin Hospital via video link.

Adelaide-based health IT solutions provider LogicPlus has been chosen to host and support the OBERD medical outcomes-based research database software for the Australian and the New Zealand markets.
OBERD is a software platform predominantly used by orthopaedic surgeons to track patient progress and recovery after surgery using patient-reported outcomes, and to use the data gathered to improve practice and for medical research.

Customer experience and patient flow management software specialist NEXA is hoping to announce several new contract wins with landmark hospitals in the near future as it gears up for an east coast roadshow promoting the Q-Flow solution it distributes in Australia from global firm Q-nomy.
NEXA has several notable installations at hospitals including the Royal Children's, the Royal Melbourne and the Peter MacCallum Cancer Centre in Parkville, at the new Blacktown Hospital in Sydney, in the outpatients and paediatrics departments at the Gold Coast University Hospital and at the Prince Charles Hospital in Brisbane.

ACT Health is looking for a supplier of medical transcription on a fee for service basis to handle excess demand as it rolls out Winscribe Text version 8.1.
Winscribe won a $300,000 tender last year to implement its medical reporting and document management solution for ACT Health, which currently uses a number of outsourced transcription services to back up its central transcription service.

Queensland's Darling Downs and West Moreton Primary Health Network (DDWMPHN) has launched a free after-hours service providing GP consultations delivered by Telstra Health's ReadyCare telehealth joint venture.
The service is available to all people in the large catchment area, including vulnerable people in the main cities of Toowoomba and Ipswich as well as those in rural areas. The PHN is also piloting an after-hours diabetes service involving face-to-face consultations in Toowoomba and remote consultations by phone and Skype to the rest of the region.

Health Informatics New Zealand (HiNZ) has issued a call for papers for its national conference in November, also announcing leading eHealth researchers Johanna Westbrook and Siaw-Teng Liaw as keynote speakers.
Dr Westbrook, director of the Centre for Health Systems and Safety Research at Macquarie University in Sydney, will ask the pertinent question of whether IT works in her talk on understanding the impact of IT in complex adaptive healthcare delivery systems.

The huge scope and complexity of the health and aged care payments IT systems that the government says are in need of replacement have been revealed in a request for information (RFI) issued yesterday, describing the first of two stages in a mammoth project that aims to have some elements up and running in less than two years.
The new Digital Payments Platform will cover Medicare, aged care and veterans payments covering 600 million transactions worth approximately $50 billion a year, including $21.4b for the MBS, $10.9b for the PBS and $13.2b for aged care.

A report of the evaluation carried out last year by consulting firm Siggins Miller of the two trials of an opt-out approach to the My Health Record is still being considered by the government, with no decision made as yet on a national roll-out, the Department of Health says.
The report was submitted to the department last year with an expectation that a decision by the government would be made in the first part of this year.

Waikato District Health Board, the NZ Telehealth Forum and Spark are holding an after five event at WINTEC on March 21 to demonstrated the region's virtual health care capabilities.
Waikato DHB has pioneered the integration of virtual technologies with acute care provision in New Zealand, launching a virtual DHB initiative, later renamed SmartHealth, in association with US telehealth platform HealthTap and with the support of Spark, in May last year.

Best Practice Software has appointed former Optus executive Janet Whitmore to a newly created role of general manager, customer and commercial, joining the company's founders, Frank and Lorraine Pyefinch, and chief operating officer Craig Hodges in a new four-person executive team.
Ms Whitmore had a long career with the telecommunications provider in a number of roles, including IT general manager for its mobile, consumer, and small to medium business units and as head of IT systems and services, where she helped develop a suite of business and mobile application units.
General practices will soon be able to offer patients a read-only summary of their medical record on their phone or iPad through Precedence Health Care's MediTracker app, which is set to begin rolling out this month to all Independent Practitioner Network (IPN) medical centres as well as any practices using MedicalDirector, Best Practice or Zedmed.
MediTracker can extract data such as current and past history, current medications, adverse reactions and immunisations from the GP clinical information system and present it in summary form through the patient app, also allowing patients and GPs to upload and graph measurements such as blood pressure, blood glucose and cholesterol, and for all members of the patient's care team to see up-to-date data in real time.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending March 5:
Moving past the EHR interoperability blame game
New England Journal of Medicine ~ Julia Adler-Milstein ~ 22/02/2017
The substantial increase in electronic health record adoption across the nation has not led to health data that can easily follow a patient across care settings.
InterSystems wins multi-million pound Liverpool joint-EPR tender
Digital Health News ~ Laura Stevens ~ 02/03/2017
Three Liverpool trusts have picked InterSystems as their preferred electronic patient record supplier, potentially winning the US company its first global digital exemplar customer.

It's always fun to watch senators on the government side of the benches squirm under the questioning of their opponents at the carnival that is Senate estimates, where the usual power structure is reversed and normally obscure parliamentarians can have their day in the sun. After all, this is where Bronwyn Bishop first made her mark back in the Hawke-Keating years and look how well that turned out.
This week in the Senate, we were served up an absolute treat as NSW Senator Fiona Nash fidgeted and fussed through a couple of hours of intense questioning by the Greens' Richard Di Natale and Labor's Murray Watt over the delay to the roll-out of the National Cancer Screening Register (NCSR). Not that Senator Nash had much to say for herself, with Department of Health secretary Martin Bowles and Commonwealth chief medical officer Brendan Murphy taking most of the heat.

The Australian Digital Health Agency (ADHA) has set up a core clinical stream as part of its work program for the coming year, adding new programs to embed telehealth and support the Health Care Homes trials to existing programs for secure messaging, medicines safety, and connecting pathology and diagnostic imaging providers and reports to the My Health Record (MyHR).
According to ADHA's corporate plan for 2016-17, released today, some of the highlights of the year will be connecting five public pathology labs and five public diagnostic imaging labs, as well as two each from the private sector, to the MyHR. eHealth NSW has also announced it will begin sharing pathology results with the My Health Record in addition to NSW Health clinicians through its HealtheNet portal some time this year.

Taxpayers will fork out at least an extra $13.5 million for a new fee for pathologists to continue providing the conventional Pap smear test in addition to the new item number for liquid-based cytology until the delayed National Cancer Screening Register is up and running in December.
Department of Health officials told a Senate Estimates Community Affairs legislation committee in Canberra this evening that extra costs will also be borne by the Department of Human Services for continuing with the national bowel cancer screening program until the NCSR is launched, six months after its promised go-live date.

The organisation representing vendors of software for the aged care industry is looking forward to renewing old connections in the eHealth sector as it joins up with the wider health IT industry, following last week's announcement that it would merge with the Medical Software Industry Association (MSIA).
Only one dissenting voice was against the plan to merge the Aged Care Industry Vendors Association (ACIVA) with the MSIA, ACIVA interim president Craig Porte said, with most hoping a stronger, united industry will hold aged care in good stead with the powers that be.

Brisbane North PHN and Metro North Hospital and Health Service (HHS) have formalised their long-standing partnership by launching a new alliance and are currently working on a transition of the region's clinical pathways program from Map of Medicine to the Canterbury HealthPathways tool.
Brisbane North PHN – then known as Metro North Brisbane Medicare Local – and Metro North HHS pioneered the use of Map of Medicine in Australia back in 2012. The tool was first developed in the UK in 2001 and was at one stage distributed in Australia by MedicalDirector.

Philips Australia and New Zealand made a bit of a splash in the eHealth arena last year with two innovative local projects: a telehealth-enabled integrated care program with West Moreton Hospital and Health Service (HHS) called MeCare, using Philips' eCareCoordinator platform and eCareCompanion app; and a pilot project with Macquarie University's MQ Health and the US-based Emory Healthcare to provide remote monitoring of intensive care patients in the US by Australian-based clinicians using Philips' eICU technology. We spoke to Philips ANZ managing director Kevin Barrow about different approaches to monitoring the deteriorating patient.

Queensland Health has issued a request for proposal for a change management partner to help the 90,000-strong organisation begin a move from its 20-year-old, heavily customised SAP enterprise resource planning (ERP) solution to a contemporary SAP finance platform, billed as a 'once in a generation' opportunity to contemporise financial administration across Queensland Health.
The $100 million Financial System Renewal (FSR) project was identified in the $1.26 billion eHealth investment strategy in 2015 as one of four 'high risk' priority systems, along with the replacement of the similarly aged patient administration system known as HBCIS, the pathology system renewal – which has gone to tender and is expected to be awarded soon – and the roll-out of electronic medical records.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.