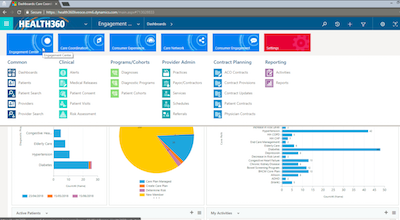
DXC Technology has signed up the first customer to use its new Health360 customer relationship management (CRM) tool, and is now looking at the private hospital and public sector markets in Australia and New Zealand to assist the local sector's move to value-based care.
Health360 is a health-centric adaptation of Microsoft's Dynamics CRM platform and uses FHIR-based APIs to exchange data with hospital electronic medical records and patient administration systems and with wearable devices. The company is also currently working on a connection to Australia's My Health Record system.
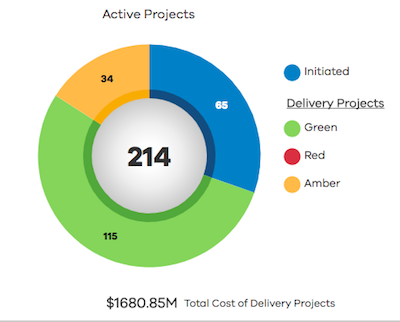
An audit of the Victorian government's ICT dashboard has found the initiative has improved the transparency of public sector ICT projects, but timeliness and completeness of information was an issue for some agencies, including the Department of Health and Human Services (DHHS).
The Victorian Department of Premier and Cabinet (DPC) launched the dashboard in March 2016 following a recommendation from the Victorian Auditor-General's Office (VAGO) that projects valued at over $1 million should be publicly reported.

Telstra has refused to comment on the future of its Telstra Health assets despite announcing a huge reorganisation of its telecommunications business today, which includes setting up a separate division to manage core infrastructure in a signal the company may sell this off once the NBN roll-out is complete.
Called Telstra 2022, the strategy will see thousands of jobs go and a huge reduction in the number of plans it offers consumers and businesses, along with a focus on productivity and attempting to monetise up to $2 billion in existing assets over the next two years.

The Australian Digital Health Agency's chief clinical information officer, Monica Trujillo, is leaving the agency after two years in the role.
Dr Trujillo was appointed Australia's first ever chief medical information officer (CMIO) during her time with UnitingCare Health in Queensland, where she was in charge of clinical engagement during the roll-out of the country's first digitally integrated regional hospital, St Stephen's at Hervey Bay.

Sydney's Liverpool Hospital will undergo a massive redevelopment over the next eight years, part of a $740 million plan to build a health, research and education hub for innovation and emerging technologies announced in today's NSW state budget.
eHealth NSW will receive about $115 million this year for clinical ICT initiatives that have already been announced in previous years, including $48.3m of the $236m allocated over six years for digital patient records, $62.8m from the $286m over nine years for the whole of system digital platform, and the final $4m of the $13.7m allocated to the HealtheNet pathology results repository in 2016.

The CSIRO's Yogi Kanagasingham was named Achiever of the Year at the WA Information Technology and Telecommunications Alliance (WAITTA) Incite Awards at the weekend for his stellar work over many years for the CSIRO Australian e-Health Research Centre, including the development of the Remote-I retinal imaging technology for diabetic retinopathy.
Perth-headquartered online appointment booking service HealthEngine took out the Dr Mal Bryce WA Tech Company of the Year award, named in honour of former WA deputy premier and ICT industry stalwart Mal Bryce, who died earlier this year. HealthEngine was also inducted into the Hall of Fame.

Australia's leading secure messaging and clinical software vendors have successfully proven they can securely exchange electronic referrals and discharge summaries between a range of different systems in the real world, in what is a major breakthrough for interoperability in the healthcare sector.
The Australian Digital Health Agency-backed trials are in the final stages of testing, with participants expected to be able to send production messages this week. The two consortia operating the proof of concepts are also finalising a federated search capability using FHIR-based APIs so healthcare providers can search for electronic addresses across the healthcare sector.

Pulse+IT's weekly round-up of international health IT news for the week ending June 17: Skepticism over AI revolution, smartphone malaria test, smartphone urine test, mobile strategy decline, Apple relies on FHIR, cyberattacks on imaging systems and medical devices, trust in NHS, UC San Diego joins Open Notes
Is AI set to transform healthcare? Not according to CIOs
MedCity News ~ David Lareau ~ 10/06/2018
Not surprisingly, these same CIOs are simultaneously skeptical about the ability of our current IT systems to deliver the top-quality, accurate and usable data that AI solutions require to perform their algorithmic magic.

The Queen's birthday long weekend languor seemed to grip the Australian health IT industry this week and it turned out to be a bit of a slow one, but the weekend itself was spiced up somewhat by a rather fascinating article in Fairfax newspapers on Saturday that had a lot of us agog.
That was the bad review saga, in which it was revealed that online appointments booking service HealthEngine had been editing customer reviews of practices on its site to such a degree that negatives were not just deleted, but sanitised to the point they became positives.

The Health Informatics Society of Australia has won its bid to host the international congress on nursing informatics in 2020, which will be co-located with the 2020 Health Informatics Conference (HIC 2020) in Brisbane.
HISA CEO Louise Schaper said NI 2020 would be a rare opportunity to learn from and network with nurses and midwives at a global level in digital health.

A study into the use of Abbott's i-STAT device for point-of-care testing in remote health centres in the Northern Territory has found it provides clinical and financial benefits, including the potential to save over $20 million a year after costs.
The Flinders University study, funded by the Emergency Medicine Foundation, assessed both the medical and cost benefits of using on-site pathology testing for acute medical care in six remote health clinics in the NT over six months in 2015.

Clinical and practice management software vendor Best Practice Software has launched the Indigo release of its Bp Premier solution, promising significant management and clinical enhancements.
Changes to the management modules include the introduction of Tyro bulk billing, additional support for multi-location sites and improvements to the Medicare Online module.

The Australian-developed TurboGrouper clinical coding and grouping software solution has this week successfully achieved an interface with DXC's webPAS patient administration system, and there are now plans to take on dominant clinical coding and grouping leader 3M in the local market.
Developed by Sydney-based Eurofield Information Solutions (EIS), TurboGrouper also interfaces with DXC's i.PM and promises powerful search capabilities and an easy-to-use interface to allow coders to quickly select codes with greater accuracy and efficiency at a lower cost.

Sydney's Health Language Analytics (HLA) took out the Premier’s award for public sector innovation at the NSW iAwards last week for its Horizon clinical natural language processing (NLP) technology, which has been deployed at the NSW Cancer Institute, the Sydney Adventist Hospital and by the Melbourne East General Practice Network (MEGPN).
Horizon is also being used by the California Cancer Registry to separate reportable pathology reports from non-pathology reports and extract clinical concepts from unstructured text.

Auckland-based telehealth provider Doctor2Go has teamed up with Napier's Westshore Pharmacy to provide in-store access to video consultations with a doctor for patients unable to see their regular GP, with plans to extend it to four other pharmacies.
The idea is not to replace regular GPs but to fill a gap for patients in the Hawkes Bay area who are unable to get an appointment at their medical centre within 24 hours, the company says.

Virtual care teams for patients with high health needs, a national “Patients Like Me” social media platform, a trial of the Open Notes project in Australia and a text/image messaging system for emergency care providers are some of the ideas put forward for the digital health test beds being organised by the Australian Digital Health Agency.
The ideas are in a new report released by the Consumers Health Forum in association with the George Institute for Global Health following a roundtable held earlier this year. The Going Digital report aims to provide guidance on using digital health to support four sectors: chronic disease, residential aged care, emergency care and end of life care.

The Queensland government has allocated an extra $154.7 million over two years in today's state budget to extend its specialist outpatient strategy, which includes work on an integrated electronic referral project and developing a platform so patients can book their specialist appointment online.
The strategy was funded to the tune of $361.2 million in the 2015-16 budget and has already achieved some goals, including giving GPs access to their patients' hospital medical records through The Viewer.

Online appointment booking service HealthEngine has removed patient feedback from its site following revelations that it so heavily moderated some comments that they appeared positive rather than negative.
Fairfax Media last week revealed it had been able to see the original reviews using the website's HTML code, showing that in addition to editing out individual doctors' names, many negative comments were also deleted.
HealthEngine launched the practice recognition program in 2015 and made it clear at the time that it was not a doctor rating site and any negative feedback would not be published but instead sent to the practice to help improve performance.

Pulse+IT's weekly round-up of international health IT news for the week ending June 10: Medisafe first Apple off the tree, safety mark for health apps, founder defends GP at Hand, another member of the Clan, Imprivata authentication tool, $352m Teladoc deal, telemedicine trends, Watson Health layoffs
Inside Apple's integration with Medisafe, the first test of the Apple Health Records API
MobiHealthNews ~ Jonah Comstock ~ 06/06/2018
The announcement that Apple would open the API for Health Records in iOS 12 will likely spawn a whole host of integrations with digital health companies in the coming months.

One of the biggest stories this week for the technology community was Apple's Worldwide Developers Conference (WWDC) in San Jose, where in addition to previewing its new macOS and iOS, Apple announced that it was opening up its Health Records APIs to third-party developers.
Apple first launched this app back in January, revealing it has been working with EMR vendors on the Argonaut Project to use the FHIR standard to develop APIs that can allow different systems to talk to each other. This involved a restricted list of vendors and 12 healthcare organisations, which has now increased to over 50, all in the US.
Medical practice management and clinical software vendor Shexie is set to launch a new web-based appointments app for its Shexie Platinum users, which will allow doctors to view their appointments on their phone, tablet or computer while out of the office or doing in-hospital visits.
The Sydney company is also planning to release a new patient portal in the next month or so, which will allow patients to fill out their demographic details and past medical history on a tablet while waiting to see the specialist, or to do so from their home computer when booking an appointment.

The lack of a suitable IT system means New Zealand will delay the full implementation of the human papillomavirus (HPV) test for cervical cancer screening until at least 2021, the Ministry of Health says.
The change from liquid-based cytology screening to the HPV test was announced in 2016 but like the National Bowel Cancer Screening Program, the new program has been beset by IT issues.

NSW Health has gone live with a statewide Wireless Core capability in a number of its agencies and is now rolling it out to local health districts (LHDs) and specialty health networks, part of a long-term plan to enable mobility, allow for secure Wi-Fi roaming across the state and to prepare the system for integrated medical devices and the Internet of Things (IoT).
Once fully deployed, the Wireless Core will allow all 160,000 NSW Health staff to connect seamlessly to Wi-Fi. It will also support the expansion of telehealth, including the state telestroke service, as well as extending the implementation of the My Food Choice system, which means food service assistants can use tablet devices rather than the old paper system to order patients' menu choices just hours before they are delivered.
Along with the Aruba ClearPass platform for authentication, profiling and network access control, some of the key elements of the platform are the state's existing Wi-Fi networks, statewide Active Directory and the Health Wide Area Network (HWAN). The latter has been rolled out to all rural and regional LHDs and is currently being implemented across metropolitan areas.

Queensland Health aims to have 80 per cent of hospital patients treated in a digitally enabled facility by 2020, with an ambitious target to roll out the digital hospital version of its integrated electronic medical record (ieMR) to 27 hospitals by the end of that year.
The digital hospital solution, which first went live at Brisbane's Princess Alexandra Hospital in November 2015, is also live at Mackay Base Hospital, Lady Cilento Children’s Hospital, Logan, Beaudesert, Redland and QEII Jubilee hospitals along with the Wynnum Manly Community Health Centre Gundu Pa, which offers allied and mental health services as well as a 24-hour primary care centre.

Practice management software vendor Best Practice has provided users with a sneak peek at its upcoming Indigo version, which prepares the groundwork for the full Indigo Service Pack 1 (SP1) containing the much-anticipated Best Health app.
Indigo, which will be available as an upgrade to Lava in the next few weeks, contains a number of enhancements, including improvements to visibility of confidential material from past visits, a new patient photo field that can attach photos to letters, a new subpoena tool and improvements to reminders and results, including a graphing functionality.

A survey of over 2800 Australians who have visited a GP recently has found that while they would like their doctor to use more digital tools to improve the patient experience, top of the list of desires was printed factsheets explaining their condition and how to manage it.
The survey, carried out by practice management software vendor MedicalDirector in association with online appointment booking service HotDoc, found that 70 per cent of respondents expected better use of digital tools, mobile technology and the internet from their GPs, in particular the ability to book an appointment online, receive a text reminder of an upcoming appointment and to receive test results and diagnoses by text, email and phone.

The ACT government has allocated $11.324 million over four years to replace the existing Kestral laboratory information system with a cloud-based solution.
ACT Health is expected to release a tender this year for the system, which it says will support the entire process of pathology services, from ordering and specimen collection through to testing, validation, reporting and billing.
Yesterday's territory budget also included the provision of $190,000 this year to continue to support the HealthPathways clinical referral portal for GPs, as well as $9.5m for health ICT upgrades, including the replacement of its purchasing and inventory control system and its hospital clinical communication system.

Melbourne's Royal Children's Hospital has issued a tender for an infrastructure platform to support a planned uplift of its electronic medical record and Orion Health's Rhapsody integration engine, which is being rolled out at the four Parkville precinct hospitals as a replacement for JCAPS.
RCH first went live with its Epic EMR in April 2016 and its three neighbours at Parkville – Melbourne Health, the Royal Women’s Hospital (RWH) and the Peter MacCallum Cancer Centre – were recently awarded $124 million to implement their own end-to-end system that will leverage the system RCH currently has in place.

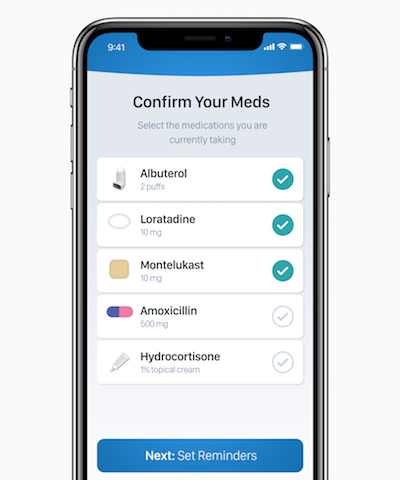
Apple has opened up its Health Records API to third-party developers in the US, allowing them to develop new apps to add to the developing app library being built by Apple that can directly access medical records held by approved healthcare providers such as hospitals and GPs.
The Health Records app, which is available only to US consumers at the moment, uses the FHIR standard to interface with EMR vendors such as Cerner, Epic and athenahealth. It was launched in beta form in January with a full release in iOS 11.3 in March, with 39 different health groups participating.
The FHIR APIs were developed as part of Project Argonaut, an Australian version of which has been established this year to localise the technology. Apple is also using OAuth 2.0 to allow users to authenticate once and create an enduring connection to the EMR APIs.

Telstra Health has been paid less than $11 million of its $200 million+ contract with the federal government to build the National Cancer Screening Register (NCSR) because the company has missed several milestones, according to Department of Health officials.
The register, which was originally due to go live for bowel cancer screening in March 2017 and for cervical cancer screening in May 2017, is still not complete, with three of the eight states and territories including Victoria yet to fully migrate data from their existing cervical cancer screening registers to the national system.

The UK-based developers of the Map of Medicine clinical pathways tool have decided to withdraw it from the market, with its referrals and sidebar tools withdrawn from sale on March 31 and its overall pathways map to cease on June 30.
Map of Medicine was originally developed in 2001 by University College London and the Royal Free Hampstead NHS Trust to outline clinical pathways and improve the quality of referrals. It was integrated into UK GP practice management systems Emis and TPP, and was also used in New Zealand and to a lesser extent Australia.

Pulse+IT's weekly round-up of international health IT news for the week ending June 3: University College London, Kaiser Permanente trying out AI, Withings back in founder's hands, device an Alexa for clinical notes, FDA and medical software, NHS data opt out, $7b offer for PMS vendor athenahealth
University College London Hospital explores AI possibilities
Digital Health News ~ Hannah Crouch ~ 29/05/2018
University College London Hospital (UCLH) has announced a new partnership with The Alan Turing Institute to explore how artificial intelligence (AI) can support clinical decision making.
Doctor's assistant Robin Healthcare emerges from stealth mode
MobiHealthNews ~ Laura Lovett ~ 30/05/2018
The device, which looks similar to an Amazon Alexa or Google Home voice assistant, will sit in a doctor’s office and draft notes from doctors' spoken conversations.

All eyes were on Canberra this week as the upper house's community affairs committee put the Department of Health and its agencies under the microscope during Senate budget estimates, but it turns out it was in the lower house where the real fireworks were about to go off.
Long-term eHealth watchers have become used to estimates hearings being quite bruising affairs, particularly when it comes to the tortured progress of the PCEHR/MyHR over the last seven or so years. But it was a much more agreeable atmosphere this week when Australian Digital Health Agency CEO Tim Kelsey fronted up with chief operating officer Bettina McMahon, core systems head Ronan O'Connor and chief medical adviser Meredith Makeham.

Melbourne's IP Health has completed an integration project for the Victorian Comprehensive Cancer Centre (VCCC) that means clinicians can access combined cardiac ultrasound images and reports generated from GE Healthcare’s ViewPoint 6 system through Carestream’s vendor neutral image viewer Vue Motion or IP Health's Verdi clinical workspace.
IP Health rolled out Verdi at Royal Melbourne Hospital, the Royal Women's Hospital and the Peter MacCallum Cancer Centre last year to support the Parkville precinct hospitals' integration strategy.

Melbourne EMR vendor Global Health has completed implementations with ACT Health's justice health and alcohol and other drug services divisions, along with the mental health services of Mercy Health in Victoria for its MasterCare EMR system.
The roll-outs saw the implementation of a single, shared client record across multiple departments and disciplines, using a best-of-breed approach with integration to multiple existing third-party systems and statewide reporting and community systems.

Sydney-based digital health start-up Tyde has moved out of its self-imposed stealth mode and is now gearing up for a national roll out its mobile platform, which allows consumers to access their My Health Record, link their family's health records together, manage appointments and prescription data and to receive tailored preventative health messages.
Last month, Tyde raised $3 million from private investors to support the national roll-out of the platform, which has been in trials with a number of care coordination groups aimed at supporting consumers with chronic health conditions.

Royal Philips has appointed Matt Moran as the new managing director for Philips Australia and New Zealand, as well as general manager for health systems for the region.
Mr Moran takes over from Kevin Barrow, who left Philips earlier this year.
The FluTracking online health surveillance system has expanded to New Zealand for the first time this year, with Kiwis now able to contribute to the collection of scientific data about the spread of influenza.
The system, which launched in 2006 with 400 participants and now numbers over 37,000, is a simple technology that allows volunteers to report their flu symptoms through an email survey every Monday morning.

The Victorian Cytology Service has begun uploading pathology reports to the My Health Record this week as numbers of diagnostic imaging and pathology providers connecting to the system continues to grow.
About 5000 DI reports and 40,000 pathology reports are being uploaded every week, with the public sector leading the way but the private sector rapidly catching up.

Publicly listed health IT vendor Orion Health has reported operational revenue within expectations and lower operating costs, but is remaining coy on any potential sale of part the business.
Releasing its 2018 financial year results today, the Auckland company reported operational revenue of $NZ170 million, within its guidance range, and an operating loss of $40.4m, which it says includes the lowest half yearly operating loss in four years.

Swedish medical imaging software provider Sectra and Australian radiology information system specialist Kestral have won a contract with NSW Health to build a proof of concept for a new enterprise-level RIS-PACS that may potentially be rolled out to 10 local health districts and NSW Pathology as a replacement for the current GE system.
The $750,000 contract will see Sectra work with sub-contractors Kestral and Sydney's Australian Centre for Advanced Computing and Communications (AC3) to build a proof of concept, which is expected to cover the common modalities used in radiology, nuclear medicine and cardiology.

Auckland private hospital group MercyAscot will roll out InterSystems' TrakCare electronic medical record to replace its existing patient administration and clinical information systems, backed by infrastructure support from NZ cloud provider Umbrellar.
MercyAscot runs two hospitals in Auckland – Mercy Hospital in Epsom and Ascot Hospital in Remuera, along with an endoscopy clinic in Takapuna – and has started recruiting for three project, technical and change management positions.

The Nepean Blue Mountains Primary Health Network (NBMPHN) has launched a three-year digital health strategy for its region, which it says is a first.
The PHN is no stranger to digital health initiatives, having hosted one of the two opt-out trials for the My Health Record in 2016 and being chosen as one of 10 PHNs to trial Health Care Homes.

Hospital pharmacists are now completing the medication plan in electronic discharge summaries in the majority of clinical units at the Alfred Hospital in Melbourne following a 2015 study that showed the practice was able to reduce medication errors.
The study, which was published in the Medical Journal of Australia last year and has just won the $10,000 MJA/MDA National prize for excellence in medical research for 2017, was conducted by a large group of clinicians from Alfred Health, led by chief pharmacy information officer Erica Tong.

Former AMA Victoria president Tony Bartone has been elected president of the national body, promising to fight for better ways of funding general practice and ensuring healthcare is centre stage in the coming federal election.
Dr Bartone, a Melbourne GP, said the election of a GP president would send a powerful message to government, which he said had underfunded general practice for the last decade.

Pulse+IT's weekly round-up of international health IT news for the week ending May 27: How WSJ reporter took down Theranos, why Geisinger is offering DNA sequencing to patients, Quebec patient portal, DirectTrust relationship with FHIR, $150m for meds management start-up, NHS Digital’s Citizen Identity system, digital health exemplars, inappropriate access to patient and pop star records
The reporter who took down a unicorn
The New Yorker ~ Yashar Ali ~ 24/05/2018
How John Carreyrou battled corporate surveillance and intimidation to expose a multibillion-dollar Silicon Valley start-up as a fraud.
Inside Geisinger Health System’s plan to offer DNA sequencing to patients
MedCity News ~ Michelle Andrews ~ 23/05/2018
Geisinger is prescribing DNA sequencing to patients and putting DNA results in electronic health records, a spokesperson said.

The Australian Digital Health Agency did a pretty good job publicising that fact that its CEO, Tim Kelsey, would be addressing the assembled hacks and no-hopers of the nation's media at the National Press Club in Canberra on Thursday.
Mr Kelsey gave a celebratory, forward-looking speech, outlining a brave new world of digitally enabled healthcare in which the hum and the whirr of the fax machine is finally silenced. He got a nice round of applause, a genial introduction from NPC president Sabra Lane and then a gentle enough opening question about the difficulties US doctors were finding with EMRs.
An independent report has found that Waikato District Health Board was right to end its two-year contract with US telehealth firm HealthTap, as the app proved to be a poor fit with the NZ public healthcare system, had several technological issues early on and had no interoperability with existing clinical solutions.
Waikato DHB commissioned an independent report from Ernst & Young into the SmartHealth initiative following the expenses scandal that engulfed its former CEO. The report found that SmartHealth has ended up costing $NZ25.7 million – about $8.9m more than the business case outlined – of which $15.4m went to the now dumped HealthTap app.

Letters will not be sent to all households and there won't be paid ads on national TV, but the Australian Digital Health Agency is implementing a comprehensive communication strategy to inform the Australian public about the My Health Record system and how to opt out of it, ADHA CEO Tim Kelsey said.
In an address to the National Press Club in Canberra today, Mr Kelsey said the agency was working with many partner organisations across the community to ensure that all Australians are aware of their rights to opt out of the My Health Record, but the lessons from the 2016 opt-out trials showed that sending a letter to households was not adequate.
An agency spokesperson told Pulse+IT that the campaign will include paid ads on local radio, in cinemas and print media as well as some specialist TV stations, along with social media and targeted campaigns aimed at different community groups. There is also a comprehensive campaign aimed at healthcare providers currently underway.

Staff in the general surgery wards at Christchurch Hospital have been given permission to keep using the Cortex digital patient list and task manager following a three-month trial in 2017 in advance of the wider roll-out of the app throughout the hospital's new acute services building.
The app, developed by Sense Medical in association with the Canterbury District Health Board, includes a clinical documentation system, electronic ordering and viewing of results, and a care coordination and communications channel for nurses, doctors and allied health staff.

Australian consumers overwhelmingly want ownership over and access to their health data, and while the majority are open to sharing de-identified data for medical research, they want to be asked for their consent first.
These are some of the findings from a comprehensive study released today by the Consumers Health Forum (CHF) and NPS MedicineWise, which found that consumers are more likely to give permission to share their data if they understand how it will be used and any benefits that will come from its use.

A remote telestroke service first piloted by Capital and Coast DHB that has now been permanently adopted in the Central region is being rolled out to Midland DHBs, with Northland implementing its own version and Canterbury DHB bidding to act as a hub for the South Island.
The service involves neurologists at large metro hospitals providing advice by video link to clinicians at regional hospitals, with the former equipped with x-ray image systems on 4G/Wi-Fi-capable iPads and the latter working with a portable telestroke unit from Auckland telehealth firm Vivid Solutions, which started life as the NZ TelePaediatric Service.

The Australian Digital Health Agency (ADHA) is looking to target geographical areas of high digital maturity rather than proof of concept pilot sites for its digital health test bed initiative, with a particular focus on health sector priority areas such as aged care and chronic disease management.
The test beds will also be used to work through some of the challenges facing the agency and mobile vendors wanting to develop APIs to access the My Health Record, ADHA told an industry briefing today.

The much-delayed Perth Children's Hospital (PCH) is in the middle of a staged opening before it is fully operational in early June, beginning to see outpatients last week and with plans to commence elective surgery next Monday.
The $1.2 billion hospital's emergency department will open on Sunday, June 10, when the old Princess Margaret Hospital (PMH) closes. PCH is using the iCM clinical information system from DXC that is still in use at PMH and Royal Perth.

Hutt Valley DHB chief executive Ashley Bloomfield has been appointed as New Zealand's new director-general of health, taking over from Chai Chuah, who resigned in February.
Dr Bloomfield is a medical doctor who has worked in public health, health policy and health services management, and since January has been acting as CEO of Capital and Coast DHB.

Several primary health networks are currently trialling the Digital Health Guide, following the lead of the Tasmanian PHN Primary Health Tasmania, which is now offering it to all health professionals in the state after a successful roll-out to GPs.
The guide, developed by Semantic Consulting in association with Hobart firm Healthcare Software on behalf of Primary Health Tasmania, is a searchable directory of over 500 health apps that have been reviewed and rated for their evidence and efficacy.

Sigma Healthcare is rolling out a new patient management and support program to its Amcal and Guardian pharmacies that is able to analyse patient medication history and notify the pharmacist if the patient may be eligible for additional professional services.
Called CarePro, the platform has been developed in association with Melbourne-based health data and patient insight specialist firm NostraData.
It promises to allow pharmacists to provide better advice and extra services, as well as produce pre-populated doctor referrals and patient summaries.

A nine-month trial of a text message-based self-management program developed by the National Institute for Health Innovation (NIHI) at the University of Auckland has seen participants with poorly controlled diabetes improve their HbA1c levels over usual care.
The Self-Management Support for Blood Glucose (SMS4BG) program, which provides a tailored package of text messages, has previously been shown to be appreciated by participants and to support them to manage their condition better.

Pulse+IT's weekly round-up of international health IT news for the week ending May 20: VA signs $10bn contract with Cerner, VA blasted for dodgy CIO, NHS aims for HIMSS level 7, Amazon-JPM-Berkshire delay, CT and ECG vulnerabilities, patient access to info stymied, open source imaging, MHS Genesis “riddled with errors”
VA finally pulls trigger and awards Cerner $10B EHR contract
Health Data Management ~ Greg Slabodkin ~ 17/05/2018
After nearly a year of negotiations with Cerner, the Department of Veterans Affairs on Thursday finally awarded the vendor a $10 billion electronic health record modernization contract to replace the VA’s decades-old legacy EHR system.
England to get first HIMSS 7 hospitals before year’s end
Digital Health News ~ Owen Hughes ~ 17/05/2018
NHS England will have its first HIMSS Stage 7 hospitals by the end of 2018, Will Smart has said, as he laid out his vision to offer ‘comprehensive, longitudinal care records’ for all 55 million English citizens within the next five years.

Was it bad timing or just bad luck that on the morning of the day the Australian Digital Health Agency decided to announce the date on which people could begin opting out of the My Health Record, a massive media storm exploded over what appeared to be a serious hack of Family Planning NSW's website, which could potentially have breached the privacy of thousands of people.
As it turned out, the hack exploited a vulnerability in a particular piece of software used to build websites, one of which just happened to belong to FP NSW. It was a ransomware attack of the kind that is increasingly common to all manner of industries and organisations, but which did not target healthcare, Family Planning or its vulnerable clients specifically.

People working in fields relating to health data, health information or health knowledge are being urged to take part in a census to help identify workforce shortfalls and training and career pathways, and finally define who and what the health information workforce actually is.
Organised by well-known health workforce researchers Kerryn Butler-Henderson from the University of Tasmania and the University of Melbourne's Kathleen Gray, the census is thought to be the biggest of its kind in the world in terms of breadth and depth, and has inspired a similar exercise for the New Zealand workforce later in the year.
The census, which opened on May 1 and closes at the end of the month, is an attempt to quantify and qualify the health information workforce (HIW), something that is a difficult thing to do, the researchers say. There are a few occupations that fit the common definition but others that, while involving health data, mainly involve technical or clinical roles.

NSW Health has announced that four local health districts will begin uploading diagnostic imaging reports to the My Health Record, using the HealtheNet clinical portal that also handles pathology reports from the public sector.
Mater Health in Queensland is also set to connect to the system for both pathology and radiology reports, and as Pulse+IT reported recently, Perth Radiological Clinic is the first private practice to begin uploading reports from the community sector.

Core Medical Solutions (CMS) co-founder and managing director Rohan Ward is relocating with his family to Singapore to oversee the expansion of the BOSSnet clinical information system in the region.
Dr Ward will also act as Allscripts' general manager for south-east Asia. Allscripts bought CMS, which supplies BOSSnet to a number of Victorian health services as well as Fiona Stanley Hospital in Perth, in December 2016.

The South Island Patient Administration Care System (SI PICS) has gone live at Nelson Marlborough Health, the second district health board to implement the new island-wide system following its pilot at Canterbury's Burwood Hospital.
SI PICS has been developed by Orion Health in association with the five South Island DHBs and the South Island Alliance to replace the nine non-integrated patient management systems used in the region, which include Homer and iPM. It will be implemented by the other DHBs over time.

The Australian MedicAlert Foundation has set out on a digital transformation process aimed at ensuring its members' information is able to be delivered to first responders and emergency clinicians in the right format at the right point in time.
The program will include a large body of work including projects to implement SNOMED and the Australian Medicines Terminology for clinical information in the member database, as well as a FHIR-based common data gateway.

SA Health will put on 30 temporary staff and has set up a taskforce to help improve pathology test turnaround times following delays to some test results since the introduction of the Enterprise Pathology Laboratory Information System (EPLIS) in 2017.
SA Health deputy chief executive Don Frater said the increase in turnaround times was largely due to initial data entry requirements associated with the roll out of EPLIS, which has been built for SA Health by Cerner at a cost of $29 million.
SA Health will also expedite the transition to full electronic test ordering at Royal Adelaide Hospital and The Queen Elizabeth Hospital to reduce the data entry requirement for SA Pathology staff.

The Department of Health and the Aged Care Industry IT Council (ACIITC) are planning a series of accelerated design workshops to help inform the $61.7 million worth of enhancements to the My Aged Care system announced in last week's federal budget.
ACIITC has issued an invitation for aged care service providers and healthcare professionals, including GPs, to take part in the workshops early next month.
GPs have long complained about the referral process to My Aged Care, which involves faxing or calling the contact centre or using a webform, as well as a lack of visibility of what has happened to their patient after the referral.

Melbourne's Eastern Health has rolled out an extensive uplift of its existing Cerner electronic medical record, going live with a customised ICU module, surgery and anaesthesia as well the FirstNet emergency department module at Box Hill Hospital, replacing the old Symphony ED solution that is no longer supported by Ascribe owner EMIS Health.
Eastern Health now plans to roll out FirstNet to Angliss and Maroondah hospitals, along with projects to optimise the new Millennium modules and then begin the task of replacing the organisation's patient administration system.

The Capital & Coast, Hutt Valley and Wairarapa District Health Boards (the 3DHBs) have issued an invitation to suppliers to their interest in providing a mobile electronic patient observations (MEPO) system to be used across the districts' four hospitals.
The DHBs are looking for a device-agnostic solution that can capture a range of patient vital signs, update vitals and progress notes as they are saved to the patient record and calculate early warning scores (EWS).

Former eHealth NSW chief clinical information officer John Lambert has joined DXC Technology as its chief medical officer for the ANZ region.
Dr Lambert is an intensive care specialist who worked in the NSW health system for 25 years, including 12 years as director of intensive care at Orange Base Hospital. He joined eHealth NSW as its inaugural CCIO in 2014..

Consumers will have have three months in which to opt out of the My Health Record before one will be created for them, with the opt-out period to begin on July 16 and run until October 15.
The Australian Digital Health Agency (ADHA) announced today that a national communications strategy will be rolled out to explain the opt-out process when the mechanisms are in place.
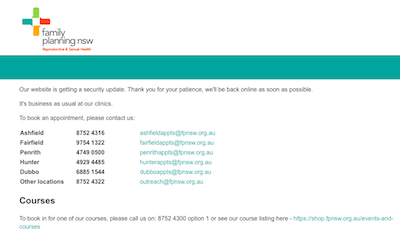
A ransomware attack on Family Planning NSW's website could potentially have compromised client names but did not affect sensitive medical records, the organisation says.
Family Planning NSW CEO Ann Brassil said the attack involved databases containing information from around 8000 clients who had contacted the organisation through its website to seek an appointment or leave feedback over the last two-and-a-half years.

The research team behind a program aimed at reducing the overprescribing of antipsychotics and benzodiazepines in residential aged care facilities has called for the program to be made available to all Australian RACFs following findings that it led to a cessation or reduction in dosage for almost 40 per cent of residents prescribed them.
The Reducing Use of Sedatives or RedUSe intervention was developed by researchers at the University of Tasmania's Wicking Dementia Research and Education Centre and uses data extraction software that automatically extracts all packed medicines from common medicine packing systems such as FredPak, Webstercare, MPS and Minfos.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending May 13: Industry loves Apple, VA decision on $16b EHR, NHS Digital data sharing, telehealth for tuberculosis, nurse snoops on ED records, Isle of Wight shares records, health IT disaster response, Allscripts buys patient engagement firm
Health systems share Apple Health Records feedback
MedCity News ~ Stephanie Baum ~ 10/05/2018
The most interesting responses were to questions focused on the potential of Apple’s health record technology, the experience so far coupled with hurdles providers face, challenges Apple faces and the likelihood of success.
Acting VA secretary to make Cerner EHR acquisition decision by May 28
Health Data Management ~ Greg Slabodkin ~ 10/05/2018
Robert Wilkie, the acting secretary of the Department of Veterans Affairs, will make an acquisition decision by May 28 regarding the VA’s plans to purchase a commercial-off-the-shelf electronic health record from Cerner to replace its legacy system, according to a senior agency official

After the massive windfall for eHealth in the 2017-18 federal budget, when the My Health Record expansion program was funded to the tune of $375 million over two years, there were comparatively slim pickings in this year's budget, although it did hold a little surprise or two.
There was a bit of money to go towards the long-term project to replace the Medicare and aged care payments systems, and another bit for My Aged Care. Apparently there was also $5 million over two years to help the National Children’s Digital Health Collaborative to develop a national digital baby book, although we missed that in all the excitement over massive tax cuts that look unlikely to eventuate. We still can't track this announcement down in the voluminous budget papers so would welcome anyone kindly showing us the way.

The federal government has released its promised framework to guide the secondary use of My Health Record system data, appointing the Australian Institute of Health and Welfare (AIHW) as the data custodian and ruling out the use of system data for commercial or non-health-related purposes or by insurance companies.
The framework details a very lengthy process that researchers wanting to access de-identified data will have to go through, which will be overseen by an independent board involving a range of independent experts.

The Ministry of Health has released regional results from the NZ Health Survey using a new Regional Data Explorer tool.
The tool allows regional data on health indicators such as obesity level, prevalence of smokers and those with mental health conditions to be compared by district health board, public health unit or regional council.

General practices in New Zealand's Pinnacle Midlands Health Network that have adopted the Health Care Home model are seeing significantly lower rates of avoidable admissions and emergency department presentations than non-HCH clinics, new figures show.
An update to a 2017 report by Ernst & Young (EY) into the HCH model has shown that in addition to previously documented benefits to patient experience, clinician satisfaction and delivery of care, there are measurable effects on ambulatory sensitive hospitalisations (ASH) and ED presentations, particularly pronounced among older people and Māori.
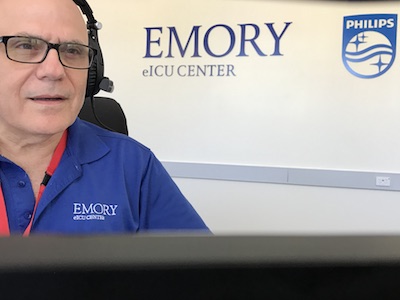
Royal Perth Hospital is hosting a remote monitoring program run by US healthcare provider Emory Healthcare that uses Philips' eICU platform to provide care for critically ill patients in Atlanta, Georgia.
Based on a pilot project held at Macquarie University Hospital in Sydney in 2016, the program involves Emory clinicians providing night-time remote monitoring of critical care patients in Atlanta during daylight hours in Perth.

New Zealand's environmental science research agency ESR is set to launch a new flu dashboard to provide near real-time information on influenza as the flu season approaches.
ESR manages the the national influenza surveillance program on behalf of the Ministry of Health and coordinates sentinel surveillance systems at hospital EDs and ICUs, general practices and through the telephone health advice service Healthline.

Sydney-based wearable device vendor mCare Digital has partnered with data analytics firm WingArc Australia to bring data analysis functionality to mCare's ConnectiveCare platform.
The technology promises to help residential aged care facilities meet the new Aged Care Quality Standards, which come into force from 2019.

Auckland-based healthcare software solutions vendor Intrahealth has appointed former HealthLink staffer Peter Mansell as its general manager for New Zealand.
Intrahealth markets the Profile suite, which includes a practice management system used by some GPs in NZ and was chosen as the preferred vendor for Canterbury's Pegasus PHO last year.

The Australian Digital Health Agency has promised to help 80 per cent of community pharmacies to connect to the My Health Record by the end of the 2018-19 financial year, with a plan to have 95 per cent connected by 2020-21.
The agency was allocated $219 million in operating expenses for the 2018-19 financial year in yesterday's federal budget, with an equity injection of $37.5m for a total of $256.8 million.
The My Aged Care system has received a boost of $61.7 million in this year's federal budget, with the stated aim of making the system easier to use.
The government has also invested over $106 million for an initial 18 months to stabilise and consolidate the health and aged care payments systems as part of an eight-year program to modernise the infrastructure.

The federal government has allocated $15.3 million in this year's budget to introduce a national electronic prescribing system for the PBS, due to begin in October 2019.
The measure will allow prescribing doctors to use their clinical software to issue an electronic prescription as a legal form of prescription. At present, the legal form of scripts must be on paper.

The Tasmanian Health Service (THS) is on the look out for a clinical utilisation review tool to help improve patient flow by assessing whether patients are receiving the appropriate level of care.
It is seeking a web-based tool that can be used across about 1000 inpatient beds in the acute, sub-acute, intermediate and mental health settings by clinical staff on a daily basis and can be integrated with existing patient information systems.

The Australian Digital Health Agency has issued a request for expressions of interest in developing some of the digital health test beds outlined in the national digital health strategy, with up to $600,000 on offer for each project.
The idea is to rigorously test digital technologies and their benefits prior to proceeding to scale them up nationally, with the first tranche to include use of the My Health Record.

The federal government is moving ahead with regulatory changes to allow PBS medicines to be prescribed without the need for a paper script, but participation will be voluntary and doctors will retain complete control over all scripts, it says.
Responding to the independent King Review of Pharmacy Remuneration and Regulation, which called for an ePrescribing system as a matter of urgency, the government said work was already underway through an electronic prescribing working group (EPWG) established in 2016 to make electronic forms of PBS scripts a legal form of prescription.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending May 6: $10b VA-Cerner deal, Ron Gutman booted from HealthTap, KRACK warning for Pyxis, Orangeworm warning for X-ray and MRI, Nokia sells Withings back to founder, WhatsApp for NHS, Windows 10 for NHS, FDA moves on software as a medical device
Cerner assesses financial hit from delay of VA EHR contract
Health Data Management ~ Greg Slabodkin ~ 03/05/2018
Cerner is feeling the financial effects of the delayed $10 billion Department of Veterans Affairs electronic health record modernization contract, according to company executives.
HealthTap has a new CEO following Ron Gutman’s ouster
MedCity News ~ Stephanie Baum ~ 03/05/2018
Ron Gutman, the founder of telehealth startup HealthTap, has been ousted from the CEO role by the company’s board of directors over allegedly intimidating and threatening behavior towards employees, in a story first reported by Recode.

We had to chuckle at a cheeky comment on our top story this week on the riches raining down on Melbourne's Parkville precinct, where after the disappointment of last year a consortium of three hospitals came up trumps in this week's state budget to the tune of $124 million to roll out an EMR.
While no one mentioned the E word you can be assured that the vendor is Epic, as the business case for funding was built to mirror the successful implementation at the neighbouring Royal Children’s Hospital and the long-held plan has always been to have a precinct-wide EMR. The executive director of the Parkville EMR project is Jackie McLeod, who led the roll-out at RCH.

Dublin-based Clanwilliam Group has added a fourth ANZ company to its healthcare technology portfolio with the purchase of Auckland's Konnect NET, which makes the SureMed solution that manages insurance company medical requests.
SureMed allows requests for health information to be sent directly to a health professional's clinical software and is integrated with the major GP software solutions, including Medtech and myPractice.
Konnect NET says all major insurers and general practices in New Zealand now manage insurance medical requests through SureMed, and the company is also using the platform to expand into Australia.

The Australian Digital Health Agency plans to go to the market in the next few months with a request for information on potentially re-platforming the My Health Record system and for the National Infrastructure Operator (NIO) after the current contract ends in 2020.
ADHA's executive general manager for core services systems operations, Ronan O'Connor, said the current system was designed and built by Accenture between 2010 and 2012 and while it is fit for purpose now, there is an ongoing need to embrace new and emerging technologies for its future.

The percentage of GPs who say they are satisfied with the way they use technology in their patient-oriented work continues to rise, although they also acknowledge there are a number of opportunities for greater use of technology, such as generating more electronic referrals, the annual RACGP survey has found.
Eighty per cent of GPs surveyed in 2017 say they are satisfied with the way they use technology up from 71 per cent in 2016 and 67 per cent the previous year.

ASX-listed imaging software vendor Pro Medicus has signed a five-year deal with Australia's largest diagnostic imaging provider to standardise the use of its Visage radiology information system across all I-MED Radiology Network practices.
I-MED has about 200 clinics across NSW, the ACT, Victoria, Tasmania, the NT and Queensland. Under the agreement, I-MED will move its Regional Imaging clinics and its Queensland practices to Visage over the next 12 months and extend its existing contract for the Victorian, NSW and ACT practices for a further five years.

Aged care software vendor AutumnCare is now offering an interface to Procura's financial management system, allowing demographic details and care-related information to be exchanged.
It has also released version 4.6.1 of its clinical system with new modules that promise to provide carers with quick access to common care tasks and reflect daily documentation features.

Ballarat Base Hospital will get a $461.6m redevelopment, Sunshine Hospital will get a $29.6m new emergency department and statewide clinical technology will get a $12m refresh from the Victorian state budget, released today.
The budget also includes $3m for planning and development to create a Parkville Biomedical Precinct, and as announced late yesterday, $124m for a new EMR for Royal Melbourne, the Royal Women's and the Peter MacCallum Cancer Centre.

Melbourne Health, the Royal Women's Hospital and the Peter MacCallum Cancer Centre will implement an Epic electronic medical record with $124 million in funding to be announced in today's state budget.
The facilities missed out last year in their bid to roll out the system used at Royal Children’s Hospital, which has seen a 27 per cent reduction in medication errors since it went live in April 2016. The bid was subsequently re-scoped.

Eight-five per cent of general practices expect to boost their technology budgets in the next two years, with more than 20 per cent expecting to significantly increase investment, a new survey has found.
Investments will focus on enhancing electronic communication channels with patients, deploying reminders for appointments and check-ups, and notifying patients of delayed appointments. A smaller number plan to invest in digital channels that allow patients to contact their GP directly or offer online portals.

ASX-listed Canberra firm Citadel Group has purchased Queensland-based practice management and billing software vendor Anaesthetic Private Practice (APP) for $2 million in cash.
Citadel, which bought oncology software specialist Charm Health in September last year for $8.2m, hopes to expand the user base of APP from mainly Queensland practitioners to NSW and Victoria, and into the public sector.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.