
The difficulties that new entrants into health IT markets face were writ large this week when Pegasus Health, the main primary healthcare organisation covering general practices in Christchurch and surrounds, finally had to throw in the towel on its venture to co-develop and roll out a new practice management system for its 90 or so members.
A few other PHOs have followed in Pegasus' path of exploring the market for a new preferred PMS that suits contemporary and future general practice. The other three big PHOs in NZ's big cities – ProCare in Auckland, Pinnacle in Hamilton and Compass in Wellington – have all gone through a preferred PMS process and all have recommended migrating from incumbent Medtech to another vendor.


Gold Coast Hospital and Health Service CIO and Robina Hospital executive director Damian Green has been named as the new CEO of eHealth Queensland, replacing Richard Ashby, who resigned in January.
The position also means Mr Green is CIO for Queensland Health. He takes over from Bruce Linaker, who has been acting in the role for the last eight months.

ACT Health hopes to go live with its new Digital Health Record in a big bang implementation at its three hospitals, followed by optimisation and additional specialty services, including a patient portal, over a four-year period.
NSW Health, meanwhile, plans to release a request for information (RFI) for its proposed Single Digital Patient Record (SDPR) at the end of this month.

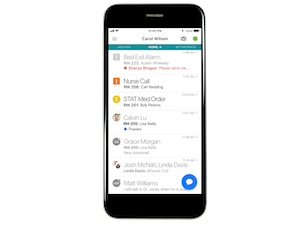
Clinical communication solution vendor Vocera has released a new app on the Australian and New Zealand markets combining prioritised calls, secure messages and alerts in a unified inbox.
Called Vina, the app presents incoming communication in order of importance, along with context that provides a meaningful picture of the patient situation including clinical events, patient status and clinician availability.

Pen CS has partnered with Sydney start-up Patient Connector to improve the referral process for GPs to specialists directly from Pen's Topbar tool.
Patient Connector launched a platform last year that allows patients with a GP referral to make a private online request for quotes from specialists outlining their fees, availability and location. It is backed by a grant from the NSW government and is being trialled in western Sydney.

Canterbury-based primary healthcare organisation (PHO) Pegasus Health has called an end to its program to develop a new practice management system for its 90 practices, saying a more competitive market meant the program was no longer viable.
Pegasus announced in 2017 that it planned to develop a new cloud-based system called Sirius in partnership with software vendor Intrahealth, building on its Profile platform, which would link to other systems such as the HealthOne shared health record and the South Island's eReferral system ERMS and be available on mobile devices.

New Zealand's market leading practice management system vendor Medtech Global has launched a chatbot called Sara to provide customer support outside of business hours, with the promise that the AI-powered bot can answer questions in real time.
Medtech says Sara will eventually be able to answer finance and sales questions, but is also a stepping-stone for Medtech to integrate AI into its software.


Healthcare information and hotline provider Healthdirect Australia went live over the weekend with a new technology platform to support its healthdirect Video Call service, replacing its former provider with Coviu, the WebRTC-based system first developed by the CSIRO's Data61.
All 5500 service providers and thousands of online clinics in hospitals, medical centres and GP practices using Video Call migrated across to the new platform on Sunday. Healthdirect Australia general manager for consumer health services Andrew Bryant said the change to the new platform had been going on behind the scenes since May.

Medical specialist software vendor Genie Solutions has partnered with men's health charity the Movember Foundation to integrate Movember’s True North digital health products with Genie.
The partnership will also make it easier for practices to submit data to the Prostate Cancer Outcomes Registry - Australia and New Zealand (PCOR-ANZ) by integrating with the registry and automating data feeds.

Icon Cancer Centre, Australia’s largest dedicated cancer care provider, has signed an agreement to roll out Synapse's Medical Billing System (Synapps MBS) across its network.
The billing system uses artificial intelligence and a rules-based engine to ensure Medicare and private health insurance claims are submitted correctly.

Pulse+IT's weekly round-up of international health IT news for the week ending September 1: Digital health IPOs, secondary use of data, cardiac rehab platform reduces re-admissions, EPS in the UK, 20m Epic records for research, Google and UCMC in court, telehealth underused, reducing sepsis deaths, Ontario EMR dashboard, Allscripts links with Apple Health Records, Zocdoc charges $3000pa
2019 is the year of the digital health IPO, but will it last?
MedCity News ~ Pete Barlas ~ 25/08/2019
After a relatively quiet IPO market, 2019 has emerged as the year of the digital health IPO with Health Catalyst, Livongo Health, Phreesia, and Change Healthcare all going public and with one more - Peloton - set to debut soon.
Most patients say they would share records for medical research
Health Data Management ~ Joseph Goedert ~ 27/08/2019
Most patients are willing to share information from their electronic medical records and biospecimens for research purposes, according to a recently completed study.

ACT Health released a tender for a comprehensive digital health record this week, revealing that the record is intended to be much more than just an electronic medical record for its three hospitals.
The ACT government has allocated $70 million over four years for its digital spend, in addition to the $11 million it has already put up for a new laboratory information system, the winning tenderer for which should be announced shortly.

The New Zealand Ministry of Health has published a set of minimum requirements for digital, data and technology services that it expects healthcare organisations to meet.
The minimum requirements are a baseline set that should be considered a minimum level of practice, the Ministry says.

More than 85 per cent of visiting medical officers at the Sydney Adventist Hospital are now using its SanCare mobile app to access and update the hospital's electronic medical record, and following its launch in 2017, the hospital is now seeing 55 per cent of all doctor activity on the EMR done through the app.
The San, one of the largest private hospitals in Australia with 500 inpatient beds, 700 active VMOs and 2000 nurses, first rolled out its SanCare EMR in 2010. Both the EMR and the app have been developed in-house for use by credentialed doctors and nurses.

North Coast Primary Health Network (NCPHN) in NSW is planning to provide access to the Digital Health Guide to GPs and allied health practitioners in its catchment, joining Primary Health Tasmania, Sydney North PHN and Gippsland PHN.
The Digital Health Guide is a web-based, searchable directory of health apps that allows GPs to 'prescribe' digital health solutions for patients electronically by sending a link to the app on the guide by email to the patient.

An app-based wellbeing assessment tool that promises to predict the likelihood of a fall with 75 per cent accuracy is being trialled at three aged care facilities in eastern Sydney before a planned national and international roll out.
The FallScreen+ app tests people aged over 60 years for health conditions that may point to a fall and features nine tests that are used to calculate an individual’s overall fall risk and identify cognitive and physical impairments that could be treated.

Northland District Health Board has joined the other northern region DHBs in rolling out an electronic charting solution for children's growth charts, with primary care clinicians able to view the charts through the region's TestSafe clinical data repository.
More than 200,000 digital growth charts have been created since the DHBs and their shared ICT services partner healthAlliance collaboratively rolled out eGrowth charts using Sysmex NZ's Eclair technology. Sysmex also developed the TestSafe system.

Patient experience analytics specialist Energesse is trialling a new tool at a NSW local health district that promises to help hospitals and healthcare services understand and improve the patient experience (PX).
The Patient Experience Maturity Evaluation (PXme) tool, which has been implemented at the Peter MacCallum Cancer Centre in Melbourne, is described as an 'experience intelligence' tool designed to diagnose an organisation's capabilities and provide decision support to clinicians, executives and frontline staff.
Energesse founder and CEO Avnesh Ratnanesan said PXme was aimed at driving consumer engagement in quality improvement and to support compliance with National Safety and Quality Health Service (NSQHS) Standard 2, 'partnering with patients', and addressing rising consumer expectations in healthcare.


The Western Australian Department of Health has issued a request for information (RFI) from EMR vendors on the feasibility and potential options for implementing a contemporary electronic medical record across the state.
A statewide EMR was one of the major recommendations of the Sustainable Health Review, which called for a phased roll-out of an EMR across the WA health system by July 2029.

BreastScreen WA has launched a new online results portal that will allow women who have opted in to receive their results electronically.
The portal provides secure delivery of the result letter through an SMS with an embedded link to within the portal.

The ACT Health Directorate has released a tender for a new digital health record to cover all public health services in the ACT, requiring full electronic medical record capabilities, integration with medical devices and consumer health monitoring devices and the ability to replace the current ACTPAS patient administration system.
The chosen digital health record must be currently implemented at another hospital system that has achieved Level 7 on the HIMSS electronic medical record adoption model (EMRAM), either for inpatients or outpatients or both.
ACT Health itself is aiming to achieve HIMSS Level 6 for the new system by 2023-24 and Level 7 by 2026-27. The new system will cover all public health services in the ACT, including Canberra Hospital, Calvary Public Hospital Bruce and University of Canberra Hospital, along with its community health centres, walk-in centres and Justice Health centres.

Pulse+IT's weekly round-up of international health IT news for the week ending August 25: Dr Google's diagnoses, McKessan pulls out of Canadian portal, Babylon's permission to expand, digital reduces deaths from sepsis, Apple health murmurs, clinical decision support v EMRs, US remains non-interoperable, UK care record downgrade, voice and privacy, health record downloads flat, AliveCor withdraws from Apple Watch
Dr Google ‘diagnoses’ 100m health concerns as GP wait times rise
Digital Health News ~ Owen Hughes ~ 22/08/2019
Benenden Health said its finding were supported by a rise in cases of “cyberchondria” – a state of medical anxiety caused by online symptoms checking and self-diagnosis.

Health IT and horrible literary allusions got mixed together this week for Pulse+IT's brains trust as we pondered the tales of two different EMR implementations in two different cities. Royal Children's Hospital in Melbourne had the best of times, our story on its Epic implementation from last week racking up a huge amount of hits on our site. It's destined to be one of our most popular ever.
While it wasn't quite the worst of times for Sydney's Northern Beaches Hospital – there has been far, far worse publicity than this, we assure you – the ill-fated opening of the hospital last year has now caught Telstra Health's EMR in its spotlight.

ASX-listed pathology, imaging and medical centre operator Healius plans to begin the five-year deployment of its new pathology laboratory information system (LIS) from SCC Soft Computer this calendar year.
It also plans to introduce eRecalls, self service check-in kiosks and a “queue remotely” app for its general practices, 95 per cent of which have now been upgraded to the MedicalDirector 3 practice management system (PMS) and online appointment booking functionality.

Trials will be held in the next year in the Blacktown-Mt Druitt region of western Sydney and the Dubbo-Coonamble region of central western NSW for the Child Digital Health Record, a national approach to harmonising early childhood data currently held in paper-based baby books.
Trials will also be held at the Mater Hospital and Cairns Hospital in Queensland of a digital health pregnancy record, which will bring together in digital form the cards carried by women to their antenatal appointments.

The Australian General Practice Alliance (AGPA) is recommending to its members that they write to the Department of Health to seek a 12-month extension on uploading patient data sets for the Practice Incentive Program Quality Improvement (PIP QI) incentive.
AGPA says it remains concerned about data governance, security of patient and practice records and a lack of clear instructions for securing patient consent for data use despite DoH having released a fact sheet (PDF) last week attempting to clarify data governance arrangements.

The New Zealand company behind the Firstcheck skin cancer detection app is opening up its company to shareholders, looking to raise $1.2 million through online equity crowdfunding platform Equitise.
Firstcheck, which allows consumers to take a photo of suspicious moles using smartphone cameras and have it checked remotely by a skin cancer specialist, has already secured $220,000 from angel investment group Enterprise Angels and Kiwi skin health clinic chain Skin Institute.

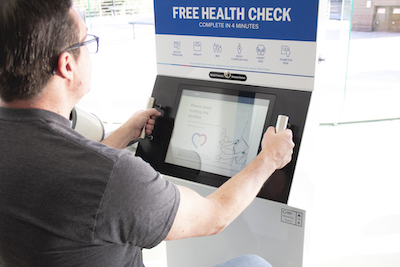
Priceline Pharmacy brand owner Australian Pharmaceutical Industries (API) has signed a five-year extension to its partnership with health measurement device vendor SiSU Health Group, which will see SiSU's health stations rolled out to more pharmacies.
SiSU's health stations offer a free health check, measuring blood pressure, heart rate, heart age, body composition, BMI, height, weight and, in Australia, diabetes risk through the Australian type 2 diabetes risk assessment tool (AUSDRISK) algorithm.

Private hospital operator Healthscope has acknowledged it made mistakes when opening Sydney's Northern Beaches Hospital last October and says it has prioritised enhancements to its electronic medical record (EMR) to focus on patient safety issues.
The acknowledgement follows a recently released report outlining problems with clinical IT by the Health Education and Training Institute (HETI) and amid strong criticism of the EMR and other clinical IT issues from the Australian Salaried Medical Officers Federation (ASMOF) in its submission to a NSW parliamentary inquiry into the hospital.

A new business case has been developed and approved for New Zealand's beleaguered National Oracle Solution (NOS) project, which has been implemented at just four district health boards after several delays.
The NOS, which began life as the Finance, Procurement and Supply Chain (FPSC) program in 2012, has also been renamed as the Health Finance, Procurement and Information Management System (FPIM).

Pharmacy group Sigma Healthcare has partnered with telehealth provider Doctors on Demand to offer in-pharmacy video consultations with GPs in rural and regional areas.
Twenty-three pharmacies from Sigma's Amcal, Guardian and Discount Drug Store banner groups are taking part in the roll-out, which will concentrate on communities with a local pharmacy but limited access to a GP.

Two general practices in Adelaide have opened as priority care centres as part of a South Australian trial aimed at diverting low-acuity cases from emergency departments.
Western Australia is also shortly to begin its trial of its new urgent care clinic network, with 133 general practices across the state participating in the pilot.

Wellington primary health organisation Tū Ora Compass Health and 20 affiliated general practices have had their websites defaced by a malicious hacker and are still offline two weeks later.
Tū Ora Compass Health acting CEO Justine Thorpe said the hack had not affected any practice management systems and there is no indication that patient information has been compromised.

Pulse+IT's weekly round-up of international health IT news for the week ending August 18: NHS spend post-WannaCry, AI accuracy in breast cancer, digital needs for GP capacity, info exchange hampers transitions of care, wearables for diabetes risk, app for GP consults, Imprivata and Microsoft IAM, AI standards needed, Allscripts settles Practice Fusion suit, customising Epic for opioid crisis
NHS trust IT spend up more than £150m since WannaCry
Digital Health News ~ Owen Hughes ~ 15/08/2019
NHS trusts have upped their IT spending by at least £152 million since 2017’s WannaCry ransomware attack, according to figures obtained through the Freedom of Information Act.
AI more accurate than docs in challenging breast cancer diagnoses
Health Data Management ~ Greg Slabodkin ~ 14/08/2019
An artificial intelligence system has outperformed pathologists in differentiating atypia from ductal carcinoma in situ—considered to be the greatest challenge in breast cancer diagnosis.

Pulse+IT headed to HISA's Health Informatics Conference in Melbourne this week, as we are wont to do, and what a smashing event it turned out to be. The focus at HIC is often on the acute care sector and, naturally, health informatics, and there was certainly plenty of that, but we were very pleased with the depth of presentations from primary care and even aged care this year.
We were also delighted to see the former chair of the RACGP's eHealth expert committee, Nathan Pinskier, pick up HISA's prestigious Jon Hilton award. Dr Pinskier, who does a huge amount of voluntary work in the background lobbying for standards and quality in health IT, joins luminaries such as Grahame Grieve, Adam McLeod, Mike Georgeff and Terry Hannan in winning the award.

eHealth NSW plans to roll out its Cerner electronic medications management (eMeds) system to 115 rural sites by the end of 2019, a large increase on the 18 sites across the six rural local health districts (LHDs) originally planned for the same timeframe.
The NSW rural eMeds project has also seen a single rural medicines formulary developed in parallel to the implementation with the aim of reducing unwarranted variation in medicines prescribed and administered in rural settings.

Melbourne's Royal Children's Hospital has seen a reduction in its mortality rate of 25 per cent since it went live with its Epic electronic medical record, and has registered similarly impressive figures for avoidable lab tests and medication prescribing and administration errors.
While the hospital is not claiming definitively that the reduction in the mortality rate is due to the EMR and may be part of an overall trend, there have been no changes to the patient population or other major intervention that can clearly account for it, RCH paediatrician and chief medical information officer Mike South said.

Patient education specialist Healthily and population health software vendor Pen CS have teamed up to offer two integrated products aimed at general practices and primary health networks (PHNs).
Healthily will provide its GoShare patient education technology integrated with Pen's CAT4 clinical audit tool and its Top Bar clinical decision support tool to allow practice staff to target specific patient cohorts with personalised content, which GPs at the point of care can also send to individual patients through a prompt from the Top Bar app.
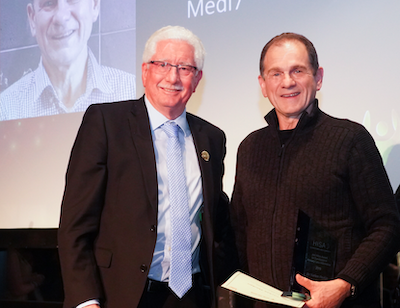
Melbourne GP and long-time RACGP expert committee on practice IT chair Nathan Pinskier has won the top award at the Health Informatics Society of Australia's annual HIC conference in Melbourne this evening.
Dr Pinskier was presented with the annual Jon Hilton award for excellence in primary care informatics for excellence in innovation across the continuum of care.

Nuance Communications plans to launch its new cloud-based Dragon Medical One speech recognition platform for the Australian market beginning next month, enabling greater efficiencies in clinical documentation and the ability to use clinicians' smartphones as a wireless microphone for dictation.
Dragon Medical One (DMO) will eventually replace the on-premise Dragon Medical Network Edition and Dragon Medical Practice Edition systems that are integrated into a number of electronic medical records and practice management systems, with mobility, better accuracy and the new PowerMic Mobile capability the key features.

Victorian-headquartered video consulting social enterprise Attend Anywhere is offering its tools and resources to public hospitals and charities in Australia for free following the end of its contract with government-owned directory and telehealth service Healthdirect Australia.
Attend Anywhere has provided its telehealth framework to public hospitals through Healthdirect since 2012. The service is a WebRTC-based system badged as Video Call and is used by a number of state health services around the country, most notably in NSW and Victoria.

Fujitsu Australia has partnered with GE Healthcare, Macquarie University and Macquarie Medical Imaging on a project to develop a solution using AI to detect and monitor brain aneurysms on scans faster and more efficiently.
The project has received a grant of $2.1 million from the federal Department of Industry, Innovation and Science and will use Fujitsu's AI and digital solutions capability along with GE's medical imaging technology.

Clinical software vendor Genie Solutions and patient engagement solution specialist HotDoc are building a joint booking solution aimed at medical specialists that will include basic triage of appointments.
Genie Solutions will handle billing and front-line support for the new functionality, which will be heavily integrated into its practice management software, while the consumer experience will be handled by HotDoc.

The Health Informatics Society of Australia (HISA) has launched Australia's first allied health informatics position paper, calling on the allied health workforce to adopt a coordinated approach to digital health.
The paper says a substantial proportion of healthcare demand is met by the allied health sector and yet the role is “poorly understood, under-utilised and largely overlooked as an area for digital reform”.

The Australian General Practice Alliance (AGPA) has called for a privacy impact assessment to be undertaken on the government's new Practice Incentive Program Quality Improvement incentive (PIP QI) to clarify concerns it has with the use of third party data extraction software and the handling of data by primary health networks (PHNs).
It has also called for a rethink of the use of PHNs to store the data rather than a single national data repository, a national sign-on contract for general practices uploads to this repository, and competitively neutral choices regarding the upload tools available.
AGPA, which represents privately owned general practices, raised an alarm about the PIP QI two weeks ago and has been consulting with the Department of Health and the PIP advisory group (PIPAG) about its concerns.

Pulse+IT's weekly round-up of international health IT news for the week ending August 11: Babylon raises $US550m, UK pledges £250m for AI, Alexa at UCHealth, GP at Hand destabilising, insurers join Blue Button 2.0, DeepMind's deep pockets, CVSHealth diabetes target, DirectTrust eyes standard for instant messaging, fractured states of American opioid crisis
Babylon Health gets $2 billion valuation with new funding that will help it expand in US
Forbes ~ Monica Melton ~ 02/08/2019
Babylon Health, a U.K.-based startup whose fast growth has been shadowed by concerns about the efficacy of its telemedicine apps, has raised $550 million in Series C funding, elevating the company to unicorn status.
Government pledges £250m for National AI Lab to improve diagnostics
Digital Health News ~ Andrea Downey ~ 08/08/2019
The programme aims to improve cancer screening and speed up results, use DNA data to identify patients most at-risk of diseases, upskill the workforce to use artificial intelligence (AI) systems and automate routine administration tasks to free up clinicians.

We must admit that yesterday's announcement by the Australian Competition and Consumer Commission that it had launched legal action against health IT firm HealthEngine was a bit of a surprise, coming as it does over a year after the online booking service was thoroughly roasted in the media for its decision to edit or delete patient reviews of practices on its site.
The main surprise was with the consumer watchdog showing a bit of bite when we thought it was due a new set of dentures. However, the ACCC recently wrapped up an inquiry into digital platforms and is keen to see consent and notification requirements under the Privacy Act strengthened, and HealthEngine may just have found itself a case study.
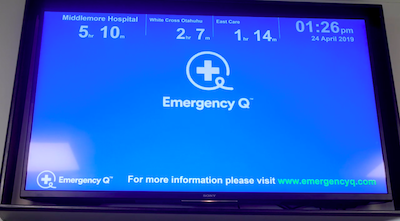
Waikato Hospital is running a six-month trial of the award-winning Emergency Q app, which has reduced emergency department patient volumes at Auckland's North Shore Hospital by 12 per cent.
Inspired by the ability to track the progress of a pizza order by developer Morris Pita, the app shows patients where the closest emergency department is and how long they will expect to wait, along with alternatives such as general practices and urgent care clinics.
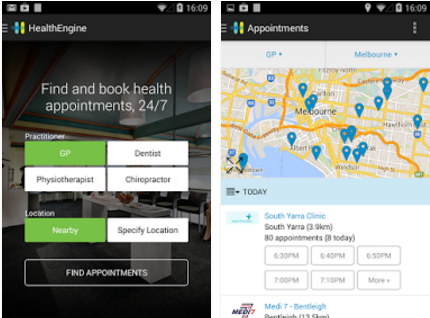
The Australian Competition and Consumer Commission has launched legal proceedings against online appointment booking service HealthEngine over its past behaviour in which it manipulated patient reviews and shared personal contact information with insurance companies.
The ACCC is claiming that between March 2015 and March 2018, HealthEngine manipulated the patient reviews of their visits to healthcare practice that the company published on its booking and directory platform and misrepresented to consumers why it did not publish a rating for some practices.

The Australian Digital Health Agency is hoping to see a 10 per cent increase in the number of medical specialists connected to the My Health Record this financial year, part of a wider strategy to increase the digital capabilities of the sector.
ADHA has been holding workshops with clinical software vendors that put in successful bids for funding through its recent co-design offer, including one held yesterday with market leader Genie Solutions.
Genie CEO James Scollay said his company planned to invest in a design-led review of its customer base to try to find a clear value proposition for specialists to use My Health Record, with improving user experience (UX) the top priority.

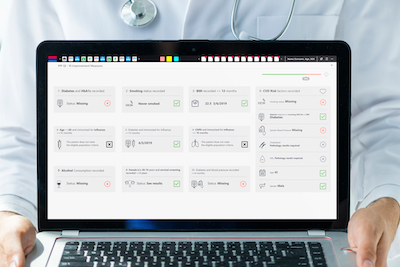
Outcome Health has released a version of its POLAR tool for general practices to support their data submission requirements for the PIP QI program.
The Melbourne-based research network is also preparing to roll out a new point of care tool called Walrus that prompts users about specific items and missing data.
The University of Sydney’s Westmead Applied Research Centre has been awarded $1 million by Google to develop a customised digital health program using artificial intelligence to reduce the risk of heart attack.
Led by cardiologist Clara Chow (pictured), the centre was set up last year in collaboration with the Western Sydney Local Health District to focus on translational research addressing chronic illness.
Professor Chow is also involved in the Western Sydney cardiology care test bed being run by the Australian Digital Health Agency to investigate the use of the My Health Record in rapid access cardiology clinics (RACC) at Westmead Hospital.

Queensland Health has delayed the planned roll-out of its integrated electronic medical record (ieMR) at Metro North and Darling Downs hospital and health services until 2021, with advanced functionality not planned to go live at Cairns HHS until 2022.
It is also rewriting its procurement plan for the long-awaited replacement of the HBCIS patient administration system (PAS), a restricted tender for which was terminated in January.

NSW Health has announced it is considering options to develop a single digital patient record (SDPR) to provide a statewide view of a patient's healthcare information.
It says the SDPR will support safe, high-quality healthcare for patients and a more consistent ICT user experience for healthcare providers.

Are you ready for your doctor to get paid for supplying your data to the government on August 1 without any need for your consent?
In an unexplained twist of federal health policy, the Department of Health through its community arm, the Primary Health Networks (PHNs), is set to gather your data regardless of your consent or not. This system is devised outside of the legislative frame of the My Health Record and has no oversight.
Primary care data solution vendor Pen CS is releasing a package of tools to support the new Practice Incentives Program quality improvement incentive (PIP QI), which is now open for general practices to enrol for.
Pen CS has integrated compliance features for the program into its existing platform as well as a new PIP QI app for Pen's Topbar tool.

GuildLink has released an update to the vaccination recording service in its GuildCare solution to allow for the Western Australian government's change to rules governing what vaccinations may be administered by pharmacists.
WA pharmacists can now administer the dTP, MMR and meningococcal ACWY vaccines to patients aged 16 years and over.

Pulse+IT's weekly round-up of international health IT news for the week ending August 4: Big tech commits to FHIR, US launches MyHealthEData, AI can predict AKI, backdoors to medical devices, Cerner picks AWS, DirectTrust standards for real-time messaging, Surescripts' war with Amazon, paediatricians and portals, free FHIR tools, voice commands for EMRs, $5b for Vista
Tech giants reaffirm support for FHIR interoperability standard
Health Data Management ~ Greg Slabodkin ~ 31/07/2019
Amazon, Google, IBM, Microsoft, Oracle, and Salesforce once again have pledged to work to advance HL7’s Fast Healthcare Interoperability Resources application programming interface.
CMS launches new API to help doctors get access to patient records
MobiHealthNews ~ Laura Lovett ~ 30/07/2019
The pilot is part of a larger CMS initiative called MyHealthEData, which is focused on giving patients more access to their medical data.

It has been years in the making and has suffered several unexpected delays, but the Department of Health's bright and shiny new general practice quality improvement incentive (PIP QI) arrived this week, and was promptly met with a chorus of disapproval from GPs.
The PIP, which replaces a handful of others and requires general practices to send quarterly reports to their primary health network (PHN) on the proportion of patients with 10 different clinical indicators, is worth the not insubstantial sum of up to $50,000 a year to practices.

ASX-listed medication adherence app developer MedAdvisor will launch into the UK market early next year, having secured its first UK pharmacy chain customer.
The company has also announced an increase in revenue over last year and hopes to improve its offering to GPs visiting nursing home patients through its Clinic Connect product.

The Department of Health has defended the design of the Practice Incentives Program Quality Improvement incentive (PIP QI) following criticism by a doctors' group, saying it was developed and agreed through an advisory group comprised of the major primary healthcare peak associations.
The PIP QI, which opened for registrations today and can be worth up to $50,000 a year for participating practices, involves practices working with their local primary health network (PHN) on quality improvement exercises, as well as agreeing to upload de-identified data about the proportion of their patients meeting 10 different measures to their PHN every quarter.

Clinical information system vendor Clinic to Cloud is launching its new software suite for general practitioners, offering a single-screen view of patient data that can be customised to the GP's individual preferences.
The Sydney-headquartered company was established four years ago with a cloud-based system for the medical specialist market and also has allied health practices on board, with approximately 4500 healthcare professionals now using the system.

A group of high-profile GPs has hit out at the Quality Improvement Practice Incentive Program (PIP QI) that will be introduced tomorrow, saying there are major concerns with the program's governance and risk management and calling for a rethink of the upload of data to primary health networks (PHNs).
The Australian General Practice Alliance has issued a paper outlining its concerns, saying that the use of intermediary organisations such as PHNs as well as data extraction software vendors introduces “significant risk and complexity regarding data governance, privacy and confidentiality”.

Victorian community healthcare provider Nexus Primary Health has moved its InterSystems TrakCare clinical information system to a cloud-based managed service.
The organisation, which includes the Wallan GP Super Clinic as well as providing allied health, mental health, disability and health promotion services to Mitchell, Murrindindi and Strathbogie shires, has taken a cloud-first systems strategy following a review of its operations.

ICT services firm Dimension Data has won a $20 million contract over two years to pilot eHealth NSW's planned Health Grade Enterprise Network (HGEN), to be offered on an infrastructure as a service (IaaS) basis.
eHealth NSW is planning to trial the network as part of the $1 billion Westmead Hospital precinct redevelopment in western Sydney, with the project used to explore different options for the procurement and management of critical ICT infrastructure.

Neurologists based at Christchurch Hospital will be available to give advice and support to doctors treating stroke patients on the West Coast following the launch of a new telestroke service.
Modelled on the hub-and-spoke service pioneered by Wellington Hospital, six spoke hospitals at Grey Base, Timaru, Oamaru, Dunedin, Dunstan and Southland will be supported by Christchurch Hospital as a hub, using dedicated video conferencing and CT image technology.

The federal government is revamping the template for consumer medicine information (CMI) leaflets, promising a shorter and better laid-out template with a one-page summary providing the most critical information.
The Therapeutic Goods Administration (TGA) plans to publish the new template shortly and will also apply it to the MedSearch app, which lets patients and clinicians find and view CMI and product information documents and save them to their mobile devices.

Best Practice Software has released an update to its Bp VIP.net package for Australian and New Zealand medical specialists, featuring enhancements to its financial system functionality.
Dubbed Ruby service pack 1 (SP1), BP's general manager of innovation and development John Rayfield said the update also has a focus on improved stability and performance.

Pulse+IT's weekly round-up of international health IT news for the week ending July 28: Livongo's big debut, US national patient ID, remote monitoring of cardiac function, EMRs find candidates for clinical trials, outsourced cancer screening failure, more AMCA victims, asking Alexa for GP appointments, Amazon threatens SureScripts, insurer taps telehealth
Livongo shares surge in market debut as digital health space heats up
CNBC ~ Christina Farr ~ 25/07/2019
Livongo Health shares surged as much as 62% in their stock market debut on Thursday, the latest sign that public investors are buying into the digital health trend.

There was interesting anecdote in one of the public submissions to the NSW parliamentary inquiry into the operation and management of Sydney's Northern Beaches Hospital, a selection of which can be found here and which include a mixture of criticism of the hospital, praise for the hospital, a bit of 'insular peninsula' whinging, and the odd suspect wearing a tinfoil hat.
One patient, who had nothing but praise for the medical and nursing staff even while recounting how one of them had allegedly punctured her artery, mentioned in passing that she had expected, now that the My Health Record was available to her, that her medical record would therefore be available to her clinicians.

Health insurer NIB New Zealand has signed an agreement with Auckland-based medications delivery service Zoom Pharmacy to improve access and adherence to medications.
Zoom Pharmacy has developed an app that provides personalised medicines information and daily dose reminders, as well as repeat and refill alerts when medications are running low.

GPs working in Sydney's northern beaches have complained about the poor communication they have experienced with the Northern Beaches Hospital since it opened late last year, including one GP who had 650 discharge summaries posted to her practice months after they were written and anecdotes that hospital staff did not know how to use its IT system.
In a public submission to a parliamentary inquiry into the hospital, local GP Caroline Rogers complained of poor communication with GPs, that they had not received discharge summaries for the first six months the hospital was open, fax machines did not work and information was not being shared.

Corum Health will make its new Clear Dispense pharmacy dispense system commercially available this month.
The company has been working on the new product suite for some years, and has now passed all the required regulatory and integrated partner approvals, it says.
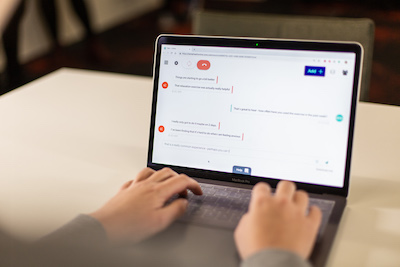
Telehealth provider Coviu has added real-time text chat functionality to its platform to help Swinburne University's National eTherapy Centre offer an extra modality for people using its Mental Health Online service.
Swinburne says text chat has proven popular with people seeking support for depression and anxiety who are reluctant to initially speak to a healthcare practitioner by video.

Sonic Healthcare has sold its 85 per cent shareholding in German laboratory automation specialist GLP Systems to Abbott for approximately $A130 million.
The technology has been installed in eight Sonic laboratories in Australia, the UK and Germany, with more planned.

Canterbury District Health Board has signed a three-year contract with Canadian technology firm Strata Health Solutions to roll out its patient flow, resource matching and waitlist management technology.
Strata's cloud-based solution will have an interface with Canterbury's eRMS eReferral system and the Orion Health electronic medical record.

Western Australia is trialling a new urgent care clinic concept that aims to encourage patients to see a GP for urgent care rather than attend a hospital emergency department.
The trial will offer urgent care appointments at general practices in the Perth metropolitan region, using an online booking service through Healthdirect's National Health Services Directory platform to capture spare appointments and show patients where and what appointments are available.

The University of Queensland is running a trial of a new fitness metric integrated into a wearable device to see if it can help people with type 2 diabetes better manage their condition.
The physical activity intelligence (PAI – pronounced 'pi') algorithm was developed by researchers from the Norwegian University of Science and Technology Faculty of Medicine based on data from the personal and family medical histories of more than 45,000 people over 25 years.

Pulse+IT's weekly round-up of international health IT news for the week ending July 21: GDPR fine for Dutch EMR snoopers, NHS tries to quell Alexa nerves, interoperability priority, Philips buys in the US, concerns over 999 triage software, PatientPing for ADT notifications, more AMCA breaches, Soom app for medical devices, NHSmail hack attempts
Patient record snooping incident leads to GDPR fine
Information Security Media Group ~ Marianne Kolbasuk McGee ~ 18/07/2019
Authorities in the Netherlands recently levied a €460,000 fine under the General Data Protection Regulation against a hospital in the Hague in connection with a data breach involving "dozens" of staffers who snooped on the electronic medical records of a celebrity.
Our top story this week on Pulse+IT was about the submission by the Royal Australian and New Zealand College of Radiologists (RANZCR) to the Australian Digital Health Agency's (ADHA) current consultation on its interoperability roadmap.
While the submission concerned the Australian policy climate, there are some very interesting ideas within it that have relevance for both the Australian and New Zealand healthcare systems and deserve serious thought.

New Zealand's South Island Alliance is running a survey of users of the Health Connect South shared health information system to see if a break-glass security layer is still required for specialist mental health, addiction and dual diagnosis patient information.
Clinicians involved in specialist mental health, addiction and dual diagnosis services do not need to break the glass to access patient records in the system, but those not working in these services do.

The Pharmacy Guild's technology arm GuildLink plans to add new functionality to its myPharmacyLink app to allow patients with diabetes to order their National Diabetes Services Scheme (NDSS) supplies directly through the app.
The NDSS product ordering feature will also allow patients to track their supply of products and receive reminders that their supply may be running low.

Community care software developer Civica Care has launched a new smartphone app aimed at care workers in the field called CarelinkGo, and has picked up three new customers in Guide Dogs NSW/ACT, disability support provider Enable WA and Great Ocean Road Health, which runs residential and community care services in the Otway region of Victoria.
Civica Care markets the Carelink suite of community care client management software, which it acquired through parent company Civica Group's purchase of Geelong-based Icon Global in August last year.

Wellington-based medical technology company Volpara Health Technologies has signed a distribution agreement with Dutch firm ScreenPoint Medical to distribute its Transpara artificial intelligence solution for mammography in Australia and New Zealand.
Transpara is described as next-generation computer-aided detection software that has been designed to help radiologists read screening mammograms by marking specific areas of the breast image as likely to be cancer or not.

The Australian-developed clinical coder training tool known as eHRoL has been updated with the 11th edition of the ICD-10 Australian modification classification, and now has over 2800 de-identified medical records for clinical coders to train on.
The electronic health records online learning (eHRoL) system has also gone international, with Ireland signing on to use the ICD-10-AM 11th edition version and an NHS trust in the UK also trialling the system.

New Zealand's Ministry of Health is considering approaching the market for a set of integration tools and partners to support improvements in interoperability and help deliver clinical information when and where it is needed.
The ministry has opened a registration of interest process for developers of integration tools and services, along with partners to help implement and support them.

The Royal Australian and New Zealand College of Radiologists (RANZCR) has outlined its top five priorities for an interoperable health system, calling for the adoption of imaging guidelines for referring doctors, an eReferrals system and shared access to historic images, as well as an ‘orderables' catalogue to standardise terminology used for radiology requests.
It has also taken a swipe at the Australian Digital Health Agency's (ADHA) focus on the My Health Record to the perceived exclusion of other digital initiatives, and at its termination of a diagnostic imaging program steering group (DI PSG) last year.

Ambulance Tasmania has issued a tender for a new secondary triage clinical decision support system to help reduce growth in demand for ambulance services for conditions better managed by primary care.
The system will support a secondary triage model for 000 callers who don't require an emergency ambulance response or transport to ED.

Pulse+IT's weekly round-up of international health IT news for the week ending July 14: DXC's Lorenzo integrates with Epic, 40 million OpenNotes, EMR algorithms for HIV, $100m telehealth program in US, NHS and Alexa team up but privacy lobby acts out, vulnerability in Zoom VC on Macs, doctors say no to patient recordings, IT teams shadow clinicians, NHS app for patient complaints, hackers attack forensic services
Royal Papworth achieves ‘first of kind’ Lorenzo-Epic integration with CUH
Digital Health News ~ Owen Hughes ~ 10/07/2019
Royal Papworth Hospital NHS Foundation Trust and Cambridge University Hospitals (CUH) NHS Foundation Trust have achieved a “first-of-type” integration in the UK, after developing an interface that allows blood test orders and results to be shared between the Lorenzo and Epic EPR systems.

This week saw a major move forward for eHealth in Australia with the news that Sullivan Nicolaides Pathology will now be routinely uploading pathology reports to the My Health Record for patients whose doctors request tests electronically.
It's not just the addition of information of real worth to patients and their record that is the breakthrough. There is also the potential spur it might give to the wider use of electronic ordering of diagnostic tests in general. While eOrders aren't new – SNP's CEO Michael Harrison told us that about 80 per cent of orders coming from GPs these days are now done electronically – it will hopefully influence specialists, who tend to order more complex tests but who also tend to use their computers to write a request and then print it out, to also send them electronically.

An app developed by medications home delivery service Zoom Pharmacy is being used in a new trial with Counties Manukau DHB to help monitor the level of adherence to medication by patients with diabetes in south Auckland.
Zoom will also deliver prescriptions to outpatients by courier to try to overcome some of the common barriers to accessing a pharmacy.


GPs and medical specialists in Queensland and northern NSW ordering diagnostic tests from Sullivan Nicolaides Pathology (SNP) will now see the resulting reports uploaded to their patients' My Health Record on a routine basis, as the Sonic Healthcare subsidiary becomes the first to offer the capability to the private sector on a large scale.
Requesting doctors must send their orders electronically from compliant practice management systems such as Best Practice and MedicalDirector to ensure the patient's Individual Healthcare Identifier (IHI) accompanies the request, which SNP says 80 per cent of GPs in the region already do.

Best Practice Software has released the Jade version of its Bp Premier practice management system featuring its new BP vendor partner network, and has also revealed it is set to integrate with Whitecoat to allow practices to use the Commonwealth Bank's new Health Claim platform.
The Jade release also has new clinical features such as updated BMI calculators, asthma care improvements and My Health Record feature enhancements, and administrative features that allow staff to view patient appointment information from the follow-up inbox.

South Western Sydney Primary Health Network (SWSPHN) is now live with its integrated real-time active data (iRAD) interoperability project, which is using Allscripts’ dbMotion solution to share patient data between general practices and other healthcare services, including hospital emergency departments.
SWSPHN first announced the project in 2017 with the intention of providing data to hospitals from GP systems and returning concise data to GPs extracted from discharge summaries in the My Health Record.

Difficulties with the electronic medical record, paging system and pathology ordering system at Sydney's Northern Beaches Hospital (NBH) compounded the staffing issues that plagued the hospital's opening, a report from NSW's Health Education and Training Institute (HETI) has found.
Junior doctors at the hospital, a public-private partnership operated by Healthscope which opened in October last year using a Telstra Health EMR, also complained separately to NSW Health that the IT system set up to provide a view into Northern Sydney Local Health District's Cerner EMR did not work, and there was no fax or internet to follow up requests.

The Victorian Agency for Health Information (VAHI) has launched a data request hub to provide easier access to health data such as the Victorian hospital data reports (HosData), mental health, alcohol and other drug treatment data and perinatal data.
The site aims to provide researchers, health services and clinicians with a single point of contract to request a range of health data and includes a live progress tracker to check on the status of the request.

Free access to dozens of standards developed by the IT-014 health informatics committee between 2004 and 2014 will no longer be subsidised by the Australian Digital Health Agency (ADHA), the agency has confirmed.
ADHA has been funding Standards Australia to provide free access to the standards online at the eHealth standards website and through Standards Australia's distributors.

Patients who have a usual GP say they receive enough information about their care but there are gaps when it comes to information sharing between providers, with almost one in four patients who attended an emergency department saying there was inadequate sharing of information back to their GP.
A new report from the Australian Institute of Health and Welfare (AIHW), based on over 30,000 responses to the the 2016 Survey of Health Care, analyses the experiences of coordination of care by patients aged 45 and over who visited a GP in one year.

Pulse+IT's weekly round-up of international health IT news for the week ending July 7: Self-registration for Apple Health Records, Theranos' Holmes blames reporter, what is NHSX? EMR messages and doctor burnout, digital to tackle rise in avoidable admissions, telehealth for post-operative care, can data be truly de-identified? EMR problems for paediatrics, Google and University of Chicago in data suit, big IPO for Livongo
Apple Health Records now available to all US providers with compatible EHRs
MobiHealthNews ~ Dave Muoio ~ 28/06/2019
Clinics and systems may self-register on Apple's website, which will allow patients with iPhones to download their records and search for their provider.
Elizabeth Holmes blames journalist for Theranos troubles
Bloomberg ~ Joel Rosenblatt ~ 29/06/2019
Holmes contends Wall Street Journal reporter John Carreyrou had an undue influence on federal regulators who concluded her blood-testing startup’s technology was a threat to patient health and forced the company to shut its labs.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.