No matter which party wins tomorrow’s Australian federal election or who holds the balance of power, there are three generation-defining issues facing the country: climate change, debt and healthcare. All three rank the highest in voters’ concerns, and detailed answers to all three have been tacitly avoided by the two major parties during this election campaign.
When it comes to health – whether that is primary care, hospital care, aged care, disability care or preventative health – the problems are stark and the answers are not easy, but they need to be confronted. The Coalition boasts of its record funding for Medicare and its response to the Aged Care Royal Commission, while the ALP conjures up urgent care clinics, voluntary patient enrolment and ensuring our elderly are properly fed. The Greens want to add dental care to the mix, and even though there is a very noticeable number of trained doctors standing for parliament, most are running on platforms concerned with climate change or political integrity rather than fixing the health system.

The New Zealand government has allocated significant funding to improve digital and data infrastructure in today’s budget, including ongoing investment in tranche two of the Hira national health information platform.
Funds have also been allocated to data and digital for the massive restructure of the New Zealand health system, as well as the Southern Health program for the new Dunedin Hospital and a population health and disease management digital capability for general practice.

WA Health needs to improve controls to better protect the personal data collected about COVID-19 positive individuals for contact tracing purposes, the Western Australian auditor-general says, following an audit into its Public Health COVID Unified System (PHOCUS) initiative.
WA Auditor-General Caroline Spencer said that while the PHOCUS system had to be rolled out quickly and succeeded in playing a significant role to support WA Health’s contact tracing efforts, she expected to find “robust access controls” in place given the sensitive nature of information it collected. Instead, the audit found a number of significant weaknesses, she said.

The Australian Department of Health will not release a report commissioned from consulting firm Boston Consulting Group (BCG) into the electronic prescription ecosystem that informed a recent tender that seeks to reduce the cost the government pays to subsidise electronic prescription exchanges.
DoH issued a tender earlier this year that looks to put a cap on the price paid to subsidise prescription exchange services (PES) – now being termed prescription delivery services (PDS) by the department – which form the basis of not just the new eScript token capability and active script list registries but also the more established barcoded paper scripts introduced over a decade ago.

Communication platform Hayylo has signed up disability services provider SensesWA to provide a dynamic digital interface for clients and their circle of support and to improve communication capabilities with care teams.
Hayylo has rolled out branded apps for a number of community, aged and disability care services through its platform, and also integrates with care management software such as Telstra Health, Procure and Carelink to enable real time interoperability and auto-synchronisation of care notes.

Clinical and practice management software vendor Best Practice Software has released a revision of its Bp Premier Saffron service pack three (SP3) containing the final changes users need to support the transition to Medicare web services.
While most software has moved over to the new system by its March 13 deadline, some BP users were given an extension until June 19. Those users must now upgrade to Saffron SP3 revision 1 and connect to Medicare web services or risk being cut off.

Several sites around Australia are about to trial a new initiative to improve communication between paramedics and hospital-based neurological teams with a locally developed digital technology platform called Zeus to improve stroke care.
The Zeus telehealth platform is able to transmit brain scans from the scene of a stroke to receiving hospitals or on-call neurologists using a smartphone app through a cloud network, as well as video conferencing between the paramedic and off-site neurologist as they make treatment and transport decisions.

Five aged care software specialist vendors have been named in the first round of the Australian Digital Health Agency’s (ADHA) aged care industry offer, which aims to help vendors to enhance their software to incorporate My Health Record functionality, aged care transfer summary documents and medication management system interoperability.
The industry offer was released late last year and contracts signed earlier this year, but details have only now been released publicly.

The Check In CBR app developed by ACT Health during the COVID-19 pandemic has been upgraded to include a new health screening tool for voluntary use by high-risk facilities, as well as a direct link to the online form to record positive RAT results.
The ACT government dropped the requirement that Check In CBR be used to check in to facilities like licensed venues, registered clubs and night clubs late last week.

A Labor government will commit $750 million over three years to implement measures recommended in the national primary healthcare 10-year plan, including the MyGP voluntary patient enrolment initiative, if it wins government this weekend.
It would also set up a $220m grant program for general practices to invest in upgrading IT systems, including to support telehealth consultations, purchase new equipment and make other improvements to ensure GP can see more patients and provide better care.

European Health Data Space, Germany’s digital health efforts ‘flailing’, 25x5 initiative to optimise EMR charting, HIMSS level 7 and better care, global clinician burnout, ophthalmology PMS hack, clinical texting, Canada’s national ePrescribing solution, US national patient identifier ban, Tennessee criminalises medical abortion by telehealth
EU ready to spend €2.5 billion on hub for health-care data
Bloomberg ~ Jillian Deutsch and Lyubov Pronina ~ 03/05/2022
The EU’s European Health Data Space aims to get citizens access to their e-prescriptions and health records online.
Germany’s digital health efforts are flailing
Politico ~ Ashleigh Furlong and Douglas Busvine ~ 12/05/2022
Germany may be known for its efficiency, but that's not true when it comes to the digitalization of its health system.

It was a very obscure little link on the Australian government’s AusTender website that first alerted technology news site ITnews and then Pulse+IT last week to the long-awaited announcement of the awarding of the JP2060 Phase 4 eHealth system replacement for the Australian Defence Force to Leidos Australia. The contract was costed at a very precise three hundred and twenty-nine million, six hundred and fifty-two thousand, six hundred and forty-three dollars and eighty cents, ($329,652,643.80), although Leidos this week in its PR said priced it at $299 million. According to ITnews the contract was signed last December, although there is no word on why it was not publicly announced at the time and was only revealed in April.

The statewide electronic medical record promised as part of Western Australia’s 10-year digital health strategy remains on the drawing board, with just $4.4 million allocated over the next few years towards planning for the initiative in today’s WA budget.
Instead, $38.1m has been allocated to rolling out the existing Opal digital medical record system at a further five new hospital sites.

Western Australia’s Joondalup Health Campus (JHC) will offer all pregnant women under its care the ability to monitor their progress at home using a smart handheld device to reduce the number of times they need to visit the hospital.
JHC, which offers public and private hospital services in a combined 722-bed service operated by Ramsay Health Care, has been running a trial of Israeli company HeraMED’s technology since early last year, initially for monitoring fetal heart rate (FHR) in low-risk pregnant women.

Regional, rural and remote aged care specialist integratedliving is the first provider to deploy a commercial application of the Smarter Safer Homes (SSH) technology to clients in their homes.
Developed by the CSIRO, SSH is an in-home monitoring and data analytics program that works by unobtrusively monitoring activities of daily living and proactively alerting for anomalies that indicate an intervention is required.

Prominent Western Sydney GP Kean-Seng Lim has joined population health solutions vendor Pen CS in the role of chief medical advisor.
Dr Lim will provide clinical governance and oversight of Pen CS, which markets software applications used for population health such as CAT Plus, a suite of health informatics technology solutions including PAT, CAT and Topbar clinical decision support.

Software solutions firm Harris Computer has finalised the purchase of NASDAQ-listed Allscripts’ hospitals and large physician practice business, rebranding it as Altera Digital Health, a business unit of Harris Healthcare.
Harris announced the purchase of Allscripts’ assets, which include the Sunrise EMR suite used by SA Health and some Victorian hospitals as well as the Australian-developed Opal digital medical record, formerly known as BOSSnet, in March this year for a price of $A950 million.


Melbourne’s Eastern Health has rolled out mobile functionality for PowerHealth Solutions’ PowerBilling and Revenue Collection (PBRC) system as part of its enterprise-wide billing initiative, which has been introduced to replace 16 different billing systems across the organisation.
The plan is to integrate PBRC with Eastern Health’s clinical rostering solution in future, which the organisation said would further improve efficiencies, including for mobile clinicians.

Leidos Australia will work with a broad consortium of software, hardware and integration specialists on the $329 million Joint Project 2060 (JP2060) Phase 4 Health Knowledge Management (HKM) solution for the Australian Defence Force (ADF).
The new system will replace the ADF’s legacy electronic health record product with a modern, patient-centric health solution, including an electronic health solution that will be delivered into the deployed environment to record the delivery of healthcare by ADF clinicians from point of injury throughout the evacuation chain into rehabilitation and recovery.

New Zealand’s market-leading practice management system vendor Medtech has launched a new integrated payments platform it is calling Medeor Pay by Link (PBL), which will become available with the next release of Medtech Evolution at the end of the month.
Medtech Medeor PBL is an online, fully integrated payment solution that enables practices to issue auto-populated invoices and receive immediate online payments.

Medical defence organisation Avant’s integrated practice management platform PracticeHub has integrated with Team Medical to allow practices to order medical supplies directly through the PracticeHub platform.
PracticeHub users can link their Team Medical Supplies account to their PracticeHub account and order PPE, rapid antigen tests, wound care consumables, vaccines and diagnostic equipment.

Former Australian Digital Health Agency executive and Cerner chief clinical information officer Monica Trujillo is leaving the EMR giant to move to Telstra Health, where she will take on the new role of chief health officer (CHO).
Dr Trujillo is effectively taking over from chief medical officer and CMIO Vince McCauley, who is leaving Telstra Health after seven years to re-focus on his external work.
Cerner’s current chief nursing and midwifery officer Michael Draheim will take on Dr Trujillo’s clinical leadership responsibilities for Asia Pacific.

US standards push, UK standards strategy, NHS digital shake-up, health app safety framework, India’s Ayushman Bharat Digital Mission, Withings goes B2B for RPM, smart watches for Parkinson’s, low retention rates for health apps, telehealth comparable to F2F, COVID-19 and data management
AMIA and HL7 join forces to promote interoperability standards
Healthcare IT News ~ Mike Miliard ~ 03/05/2022
The two-year collaboration will focus efforts to extend comprehensive standards for interoperability and specs such as FHIR across the healthcare community.
A rather peculiar tender was issued by the Australian Department of Health back in September 2021 for a review of the electronic prescribing ecosystem, with particular emphasis on the funding model. The tender was full of the usual government verbiage, talking about the need to look at “opportunities to improve the customer experience for prescribers, patients and dispensers; optimise the environment to support further scale; and to ensure the effectiveness and sustainability of the operating and funding model”. In other words, it wanted to look at cutting costs.
We hear that one of the usual suspects in the big four consulting groups won the contract to take at look at this ecosystem, saw that the department was not only funding every eScript token that a GP sent out by SMS but that it had in fact been paying for every printed script issued with a barcode for close on a decade, and decided to recommend cutting back on these subsidies.

The board of the New Zealand Medical Association has recommended that the organisation be liquidated at its annual general meeting at the end of the month.
Board chair Alistair Humphrey said in a statement that the financial situation of the association was unsustainable following two decades of stagnant membership and the accumulation of deficits that had reached the point where the union needed to dissolve or face becoming insolvent.

Royal Prince Alfred Hospital in Sydney has extended its rpavirtual service first developed for palliative and chronic care patients and then ramped up to provide care for COVID-19 patients at home to a new virtual rehabilitation program and an intensive care service for critically ill patients at Broken Hill Base Hospital in western NSW.
rpavirtual was established as a proof of concept project in early 2020, just as the coronavirus hit. It was rapidly scaled up to provide help for COVID-19 positive patients, with a 24/7 virtual care centre set up staffed by RPA nurses, with Sydney Local Health District (SLHD) community nurses also visiting patients in their homes.

A recent evaluation of the My Emergency Doctor service used by Eastern Melbourne PHN (EMPHN) shows that it has helped to cut down on emergency department presentations and ambulance trips, and also provides value for money.
EMPHN first trialled the My Emergency Doctor app in 2018 for after-hours care and then expanded it for semi-urgent and urgent after-hours care in 2019, including for people living in residential aged care facilities.

Guidelines for the use of the My Health Record in the aged care sector are nearing completion amid hopes they can improve on the ‘dismal’ uptake of the system, with official figures showing just 14 per cent of residential aged care facilities are registered for My Health Record and of those, only three per cent are actually using it.
The Aged Care Industry IT Council (ACIITC) has been working with the Australian Digital Health Agency (ADHA) on a big project looking at a range of issues for digital health in aged care, including digital infrastructure, the adoption of clinical software and its interoperability with external systems, as well as new initiatives for the My Health Record such as a transfer of care document.

The two main aged care provider associations have officially joined forces in a united front for the industry following years of discussions, following a call by the Royal Commission into Aged Care Quality and Safety for greater industry collaboration and unified leadership.
Last week, the members of Aged & Community Services Australia (ACSA), representing the not-for-profit and faith-based provider sector, and Leading Age Services Australia (LASA), formerly known as Aged Care Association Australia and representing large and small commercial operators, voted to a formal merger.

The Australasian Institute of Digital Health (AIDH) is recommending the development of a fully funded, national virtual care strategy in its 2022 federal election statement, calling on parties and candidates to support continued investment in the digital enablement of healthcare.
A national virtual care strategy is one of three themes it has outlined its ‘Shifting the dial on Australia’s transition to a digital health future’ statement. The other two cover a commitment to a digitally enabled health workforce, and investment in the infrastructure needed for a 21st century healthcare system.

The Victorian government will invest $698 million over four years in its Better at Home program to expand the care patients can access in their home in a landmark program boosted by the success of home-based and virtual care programs during the pandemic.
Today's state budge also allocates $65 million over four years to deliver an electronic mental health and wellbeing record, an information exchange platform, and an online portal to support mental health and wellbeing services.
There is a small amount going towards the safer digital healthcare for Victorian public health services initiative to upgrade the network infrastructure needed to support and deliver patient-related services such as pathology, diagnostic imaging and patient management systems.

A consortium led by technology solutions and services firm Leidos Australia has won the long-standing Joint Project 2060 (JP2060) Phase 4 eHealth system replacement for the Australian Defence Force (ADF).
The $329.6 million, seven-year contract will see the existing Defence eHealth System (DeHS) that uses the UK's EMIS practice management system replaced with a contemporary system using cloud PMS vendor MediRecords for the primary and allied healthcare requirements, telehealth specialist Coviu for the telemedicine capability and Alcidion to aggregate data from consortium partner solutions to provide a single, consolidated, longitudinal view of participant health status and history.

The University of Queensland’s Aged Care Data Compare (ACDC) project is expecting to go into operation with a data hub for aged care quality indicator benchmarking in the next few months, the first step in establishing a minimum data set for the sector.
The project aims to build tools to enable data to be exchanged between software solutions and across care settings using FHIR implementation guides for data exchange.

Health Informatics New Zealand (HiNZ) CEO Kim Mundell has stood down after eight years in the role to focus on her consulting business.
HiNZ has appointed sales and marketing general manager Kylie Williams to act as CEO from June 1 while a replacement for Ms Mundell is found.
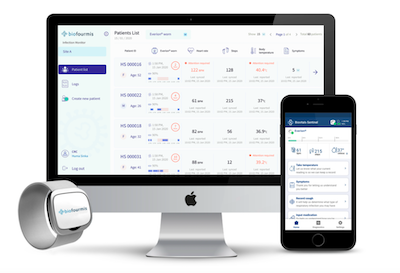
Interoperability divide in small and large practices, New York HIEs launch SMART on FHIR app, White House talks to Epic and Cerner on COVID antivirals, Emotet botnet makes a return, Singapore’s Hello Health to list on ASX, UK data sharing bill, wearable sensors and COVID vax, Biofourmis reaches unicorn status, Palanitr to build federated data platform for NHS
A fragmented EHR market is fueling interoperability divide, says ONC study
Healthcare IT News ~ Kat Jercich ~ 27/04/2022
Researchers from the Office of the National Coordinator for Health IT found substantial differences between solo practice physicians and large practice physicians when it came to data exchange capabilities.
NY HIEs launch SMART on FHIR app to enhance interoperability
EHR Intelligence ~ Sarai Rodriguez ~ 25/04/2022
The SMART on FHIR application will allow providers to access HIE information directly within their workflows, improving interoperability and data access.

Pulse+IT’s readers prefer us to stay out of politics and refrain from commenting one way or the other and we generally try to do so, but with a federal election just three weeks away and the topic of healthcare barely touched on by our leaders, it’s getting tough.
Barely a peep has come out from the Coalition about healthcare policy beyond the usual spin about record funding, guaranteeing Medicare, free medications, ‘permanent telehealth’ and so on. With health minister Greg Hunt retiring and a non-entity like former social services minister Anne Ruston to take his place, and aged care minister Richard Colbeck currently on holiday either in Coventry or perhaps even Siberia so quiet he has been, healthcare policy and funding is not getting much of a run.

St John of God Health Care has used a digital solution from Personify Care to help its Healthcare to Home post-discharge service to reduce manual screening as well as preventable re-admissions of surgical patients.
St John of God Murdoch Hospital in Perth first instituted the preventable re-admissions pilot project in 2019 to reduce the number of re-admissions through its Healthcare at Home service.

Melbourne-headquartered Lenexa Medical’s software and sensor-based solution for pressure injury prevention has been approved for sale in New Zealand.
The solution is currently undergoing a trial at Bendigo Hospital in Victoria and involves an Australian Therapeutic Goods Administration-approved solution for preventing pressure injuries in hospital and residential aged care facilities.

IT services provider Datacom has received a three-year extension to its contract with the Australian Department of Health as its prime ICT infrastructure and support services contractor.
The new contract adds to a pandemic-inspired extension in 2020, building on a five-year, $242 million contract first awarded in 2015.

Home and community nursing care provider Silver Chain is using telehealth and face-to-face visits for COVID 19-positive patients living in residential aged care facilities and private psychiatric hostels in Perth who need additional healthcare support.
Silver Chain is working with the WA Primary Health Alliance and local GPs on the initiative, which will see Silver Chain registered nurses provide care for a range of health conditions including chronic disease care, minor injuries, wound care and catheter management.

The first three modules of Dementia Australia’s mobile Ask Annie app are being subsidised for free downloads for aged care workers to help strengthen their dementia care skills.
The app, developed by Dementia Australia with Deakin University's Applied Artificial Intelligence Institute (A2I2) through the ARC Research Hub for Digital Enhanced Living, offers short, self-paced learning modules to help care workers refresh their skills and learn tips and tools to provide better care to people living with dementia.

eHealth NSW has delayed the closing date for its $10 million Health Wide Area Network (HWAN) core network refresh project for a third time.
The project is looking to upgrade the HWAN, which supports telehealth, WiFi and applications across the state, to a network as a service (NaaS) basis. eHealth NSW first built the HWAN in 2016 and currently owns and operates the network itself.

WA Health has issued two new tenders for software licences, implementation services, devices and hardware to support its digital medical record (DMR), which it says it intends to roll out across the state.
WA Health uses a mixture Allscripts’ eForms solution as well as a scanned version of paper forms, and documents from WA Health’s other ICT systems such as iCM.

Northern Health’s Virtual emergency department (ED) has added Ambulance Victoria to its triage service, allowing paramedics to use the Virtual ED service from a patient’s home and receive emergency medical advice and care.
The Virtual ED and Ambulance Victoria partnership covers the north-eastern catchment area and follows the launch of the virtual service last year for patients and GPs. It uses Healthdirect's Video Call telehealth system.

Global healthcare software giant Dedalus created a New Zealand-based development and test engineering team for its MedChart ePrescribing and medications management system in its Wellington office.
Dedalus says the team will act as a bridge to the company’s research and development capacity within its global development centres.

Rating system for health apps, Meditech’s genomic EMR solution, India’s digital health potential, Hive ransomware threat, hand-held sonography, AI aids colonoscopies, medical device security, EMR satisfaction, telehealth for veteran mental health, Epic’s Garden Plot, $4b digital health start-up over-promises and under-delivers
Rating system for health-related smartphone apps may be beneficial
mHealth Intelligence ~ Mark Melchionna ~ 20/04/2022
A rating system can help lead clinicians to a smartphone application that can benefit certain patients by winnowing the exhaustive list of available apps down to a few for clinicians to consider, according to a study published in JMIR mHealth and uHealth.

ASX-listed ResApp Health has been making some pretty big moves and pretty big claims in the last year or so for its respiratory health software apps, so it was no real surprise that a Big Pharma company has been sniffing around. What is a bit surprising in Pfizer’s bid for the Brisbane firm is the size of its offer, which values the company at $100 million.
ResApp has been around for quite a few years, having been founded in 2014 to commercialise technology developed by University of Queensland biomedical engineer Udantha Abeyratne. It officially listed on the ASX in 2015 through a reverse listing with the former Narhex Life Sciences, and since then has run some pretty impressive trials, in particular at Joondalup Health Campus in WA, into using the technology for remote diagnosis of COPD, asthma and pneumonia through artificial intelligence analysis of cough sounds. It also has a sleep apnoea app called SleepCheck that is going great guns.

West Australian surgical hospital and palliative care operator Bethesda Health Care has implemented Microsoft’s Cloud for Healthcare technology at one of its mental health clinics, using it as a patient administration system (PAS).
The Microsoft Cloud for Healthcare package brings together Microsoft Azure, Dynamics 365, Microsoft Power Platform and Microsoft 365 and uses what it calls a starter healthcare data model aligning with HL7 FHIR standards to support data interoperability.
A survey of over 250 people working in digital health in Australia has found that despite a higher proportion of women to men working in the field than in other IT sectors, women are still underrepresented in leadership and highly technical positions.
The survey also found that more men were happy to stay in the field than women, and that salaries for women in comparable positions were lower than for men.

Ambulance Victoria paramedics are now being given telehealth access to emergency department clinicians to help determine the most appropriate care for a patient in a partnership with Monash Health, Alfred Health and Peninsula Health.
The new Virtual ED service will allow medications to be prescribed and forwarded to the patient’s pharmacy and discharge summaries sent to the patient’s regular GP.

Artificial intelligence analytics and facial recognition technology developer StrongRoom AI and pharmacotherapy software solution vendor EasyDose have joined forces, aiming to provide a consolidated platform for controlled drugs to pharmacies.
StrongRoom AI provides an AI-driven controlled drug management platform aimed at reducing adverse drug events within pharmacy, hospital and aged care facility settings, while EasyDose provides a solution to streamline the daily dispensing of methadone and buprenorphine to opioid-dependent clients.

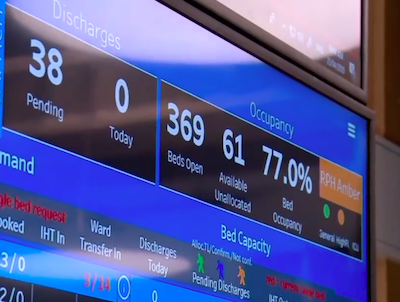
Northern Territory Health plans to upgrade the Miya platform from Alcidion that it has used for over a decade and deploy the latest version of the Miya Precision solution to support patient flow and bed management between its major hospitals and satellite health services.
The platform will also integrate with the Acacia electronic medical record that NT Health is rolling out across the territory, using InterSystems’ technology under the $259 million core clinical systems renewal program.
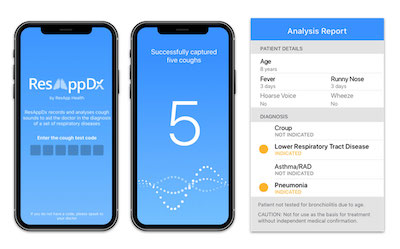
Pharmaceutical giant Pfizer has made an offer worth approximately $100 million to buy 100 per cent of the shares in AXS-listed respiratory health software developer ResApp Health.
ResApp and Pfizer have also entered into a research and development license agreement to work together on R&D for products in the field of COVID-19. ResApp recently announced it was planning a randomised control trial of its new app-based diagnostic screening tool for COVID-19.

Wellington-headquartered rostering software solution vendor Core Schedule has promoted its technical lead Cade Murphy to the position of chief technology officer (CTO).
Mr Murphy has been with Core Schedule for nearly three years. His new role will be focused on guiding the development team, improving Core Schedule’s systems and workflow, assessing new product features and developing product strategies.

The SafeScript NSW real-time prescription monitoring system for drugs of addiction is scheduled for roll out in two highly populated areas of Sydney, following the program’s launch in the Hunter New England and Central Coast Primary Health Network late last year.
The system, built by Fred IT and based on Victoria’s RTPM program, has also gone live in the Northern Sydney and Nepean Blue Mountains PHNs. It is set to go live in South Western Sydney PHN and Central and Eastern Sydney PHNs at the end of next month.

Health IT giant Dedalus has appointed former Fujitsu executive Mika Joronen as its country manager for New Zealand.
Mr Joronen previously worked for Hewlett Packard Enterprise in NZ as an account executive for government and defence, and in a similar position for DXC.

The Australian Association of Practice Management (AAPM) has put forward a proposal for funding to develop training initiatives for new and experienced practice managers to better equip them for primary healthcare reform.
The proposed curriculum emphasises training in developing integrated models of care using digital health as well as strategic information management in a primary healthcare setting and healthcare system literacy.

Online appointment booking solution vendor Healthengine has signed on with Australian Pharmaceutical Industries (API) to roll out its patient appointment management system (PAMS) at API’s Priceline pharmacies as the flu vaccination season approaches.
API’s Priceline joins Sigma Healthcare’s TerryWhiteChemmart, Amcal and Guardian banners in implementing the system, which will handle online bookings, scheduling and payment for the flu season as well as the continued COVID-19 vaccination and booster effort.

All four hospitals in Melbourne’s Parkville Precinct have received stage 6 validation in the HIMSS inpatient electronic medical record adoption model (EMRAM) assessment, with Royal Children’s Hospital also scoring stage 7 for its outpatients EMR implementation.
Royal Melbourne Hospital, Royal Women’s Hospital and Peter MacCallum Cancer Centre all completed their first EMRAM assessments last week, following in the footsteps of pioneer Royal Children’s Hospital (RCH), which was first assessed in 2017.


St Vincent’s Hospital Melbourne has launched an upgrade to the Talk to Me language interpretation app first implemented in 2015. St Vincent’s Hospital Melbourne cultural inclusion lead Monita Mascitti-Meuter explains how the original app has been improved, and how it is improving the patient and clinical experience.
Imagine this – you’re in your seventies and have recently migrated to Australia. You speak three languages, but it's a little late to learn fluent English. You make a real effort, but due to your physical ailments, you have to enter into nursing care, away from your family and into an environment where no one speaks your language.
Recognising the importance of ethnocentric care is imperative within the healthcare setting, accommodating the linguistic needs of those who are most vulnerable. However, the financial burden of requesting interpreter support over an extended period of time can be demanding. Interpreters are generally called in at vital points of care, but for the hours and days in between, residents are often left feeling lost in a foreign world.
The Australian Medical Association (AMA) has highlighted digital health technologies as one of its five pillars to build a sustainable health system of the future in its pre-election statement, calling on the next government to invest in data and technology to consolidate the gains from COVID-19 reforms such as telehealth and ePrescribing.
The AMA’s five pillars are general practice, public hospitals, private health, a health system for all and a health system for the future. Building a health system for the future, the AMA says, will require the embrace of new technology and innovation.

ASX-listed Global Health has taken a 20 per cent equity stake in Asta Swisstec Health, a Northern Territory-based company that has partnered with Philips Healthcare to provide health technology services to regional and remote Australia.
The partnership aims to help deliver digital services to people in northern Australia and in south-east Asia through the deployable healthcare module (DHM) project spearheaded by Philips, Swisstec Analytics and the Northern Territory government.


NHS England’s federated data platform, US’s Covid-era telehealth rules, trusted research environments for sharing data, California HIE, virtual GP care in Ireland, how to build a virtual ICU, EMR data for personalised care, Denmark’s digital mail service
NHS England planning to develop a £240million ‘Federated Data Platform’
Digital Health News ~ Jon Hoeksma ~ 06/04/2022
The data platform will be an “essential enabler to transformational improvements” across the NHS and will be an “ecosystem of technologies and services”.
Yes, we know we have been banging on about this for ages but this week has revealed in living colour just how ridiculous outgoing health minister Greg Hunt’s commitment to telehealth is. Despite masses of spin to the contrary, the Australian government has no intention of instituting universal permanent telehealth, and nor has it gone to Herculean efforts to institute it, as the Medical Software Industry Association ridiculously likes to tout.
The surreptitious release of the grandly titled Primary Health Care 10-year Plan – allegedly published on March 25, four days before the budget but somehow evading everyone’s notice – suggests that there are quite a lot of elements to the plan that the Department of Health wants to hide.

St Vincent’s Hospital in Sydney’s Darlinghurst has opened what it says is the first post-acute multidisciplinary COVID-19 clinic in NSW, offering services in person and by virtual care to patients who are still suffering the effects of COVID months after testing negative.
St Vincent’s has been running the ADAPT observational study following people post COVID-19 infection, aiming to characterise outcomes over at least one year of follow up to understand how people’s bodies respond to the virus.

Monash University is leading a project testing whether improved care coordination and symptom monitoring using Personify Care’s digital patient pathways can improve quality of life for people with pancreatic or oesophagogastric cancers.
The PROpatient project is funded by the Victorian Cancer Agency and will recruit patients using Monash University's upper-gastrointestinal registry across 12 participating sites, including Austin Health, Cabrini Health, Western Health and St Vincent's Hospital, Melbourne.

New Zealand’s director-general of health, Ashley Bloomfield, will step down from his role a year earlier than scheduled.
Dr Bloomfield, a specialist in public health medicine, has been the face of New Zealand’s response to the COVID pandemic.

Victoria’s Bendigo Hospital is running a trial of an Australian-developed, TGA-approved fabric-based sensor that assists clinicians by providing real-time monitoring of patient position to enable personalised pressure injury prevention.
Developed by Melbourne-headquartered Lenexa Medical, the technology uses in-built sensing capabilities and smart software for detecting and monitoring pressure injury risk.

Video telehealth platform Coviu has partnered with language services provider Ezispeak Health to integrate on-demand access to interpreters through telehealth.
In addition to GP interpreting services, the technology can be used for emergency appointments in the acute sector, having been trialled at Alfred Health.

The once troubled Weststate Private Hospital venture that plans to convert the former Townsville West State School in northern Queensland into a short-stay hospital specialising in orthopaedics and urology has added to its IT portfolio, contracting Rauland Australia to implement its Concentric Care nurse call and patient engagement platform in the 50-bed hospital.
The $60.5 million Weststate Private is understood to have contracted with Phillips Healthcare for its Tasy electronic medical record in what its proponents say will be the first fully digital day hospital in northern Australia.

Leading New Zealand digital health companies HealthSoft and Valentia Technologies have formed a long-term partnership with social enterprise Whānau Tahi to collaborate on better health equity and health outcomes for Māori.
The partners will develop a collaboration framework to enable Whānau Tahi to incorporate advanced technologies from Valentia and HealthSoft for their iwi and whānau support services.

Australia’s Heart Foundation is expanding a program it piloted last year to encourage people to get an MBS-funded heart health check from their GP using SMS recall technology to automate the process.
The Text to Detect program uses technology from patient education specialist Healthily and population health data extraction firm Pen CS. The Heart Foundation says it is the largest quality improvement program of its kind in Australian primary care.

West Australian aged care provider Bethanie is running a trial of artificial intelligence technology to collect behavioural and health data in real time using sensors installed around its residential aged care facilities.
The proof-of-concept trial will see the captured data processed using artificial intelligence and downloaded to a dashboard to give carers an insight into residents’ health and wellbeing.

Digital health training for Canadian clinicians, health IT in Ireland, flash glucose monitors for T1D, ePHR for migrants proves worth, remote pulse oximetry monitoring, medical device security, telementoring cuts admissions, US VA Cerner roll-out, Epic enters CRM market
Canada-wide initiative will prepare trainees and early career researchers to be future leaders in digital health solutions for older adults
Yahoo News ~ Staff writer ~ 01/04/2022
A new federally-funded national training platform will equip graduate students, postdoctoral fellows and early career researchers to accelerate the delivery of digital health solutions for older Canadians with complex health needs and their caregivers.

Cost of living pressures may be the name of the game in this year’s Australian federal election, but aged care and healthcare will surely play a big role. The Coalition government has been touting its healthcare cred in the lead up to this year’s budget, citing the billions spent on the COVID response as evidence of healthcare spending, along with the vast sums it can conjure for newly subsidised medicines on the PBS.
It is also touting yet again its “rock-solid commitment to Medicare”, otherwise known as the Medicare guarantee, which outgoing health minister Greg Hunt has used for years as a slogan to push back against Labor accusations of inadequate funding for healthcare and other assorted Mediscares.

New Zealand’s healthcare IT industry association NZHIT has rebranded as the Digital Health Association (DHA) in what it calls the move to the “fourth industrial revolution”.
NZHIT has been around since 2002 and now represents over 170 members, including software and hardware vendors, healthcare providers, consultancies, legal, insurance, banking, and government and regional agencies.
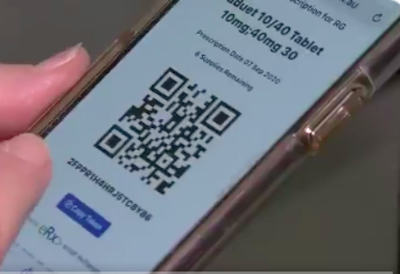
The Australian Department of Health has issued a request for tender for prescription delivery service (PDS) providers and for a single active script list registry (ASLR) provider as part of its review of the electronic prescription ecosystem.
The RFP says the department is looking to engage a single or multiple PDS providers – the current two are eRx Script Exchange and MediSecure Script Vault – as well as a single ASLR provider. The existing ASL registry is provided by Medication Knowledge, a joint venture between eRx and MediSecure.
Medication Knowledge also powers the National Data Exchange, the basis for prescription information used by the real-time prescription monitoring systems for controlled drugs of dependence that are rolling out around the country.
Telstra Health has launched a mobile app for aged care facilities that is integrated with its Clinical Manager residential aged care software to enable care staff to document and view residents’ data at their side.
According to Telstra Health, CareKeeper uses an icon-based design to help staff identify the tasks that need completing while at the resident’s side and lets them tick off the most urgent tasks as soon as they have been completed.
It is small change in the scheme of a $132 billion overall health and aged care budget for 2022-23, but the Medicare payments modernisation program, PHN-commissioned after hours programs and some additional funding for Healthdirect Australia’s national triage, assessment and referral service are the highlights for new digital health initiatives.
$107.2 million is going towards modernising the healthcare system as part of the government’s long term national health plan. This includes $72 million over four years to support phase three of the health delivery modernisation program to build a new platform for streamlining and digitising Medicare and aged care payments.

The Australian government’s federal budget was light on new initiatives for digital health, but has maintained annual funding for the Australian Digital Health Agency at previous levels to the tune of $213 million.
$3 million has been set aside to provide data linkages between the My Health Record system and the voluntary patient enrolment scheme being developed by Services Australia, dubbed MyGP. That initiative received $50.7m in last year’s budget for technology systems to support it, but confusion still reigns on exactly when the initiative will go ahead.

Sydney Local Health District is rolling out Vocera’s hands-free wearable communication devices to its emergency departments following a quick-fire trial in its ICUs during the Delta outbreak of COVID-19 in September last year.
Royal Prince Alfred and Concord hospitals have adopted the new technology in their EDs as well as ICU, with Canterbury Hospital’s ED in the process.

Waitematā District Health Board plans to roll out the Pinga online appointment booking system at North Shore and Waitakere hospitals, initially in its cardiology clinics followed by a wider roll-out between April and December across most outpatient clinics.
Pinga, developed by technology firm Sorsix and distributed in New Zealand by Aceso, is a modular, cloud-based solution that in addition to patient appointment booking, includes roster and scheduling, eReferral management, patient reminders, operational dashboards and an integrated telehealth service.

The New Zealand Ministry of Health has released a request for proposal for the replacement of BreastScreen Aotearoa’s (BSA) ICT solution, looking for an end-to-end solution that extends the existing Salesforce-based National Screening Solution (NSS) as well as the provision of a new radiology information system to replace the legacy solution.
The ministry is seeking to replace the Concerto BreastScreen (cBS) that Orion Health has delivered since 2005 for New Zealand’s eight lead providers of breast screening services, which all use a different instance of cBS.

Victoria is considering setting up a managed gateway for electronic referrals into the public health system in advance of full interoperability between secure messaging services.
While the other states and territories are increasingly looking at a single solution for managing eReferrals, Victoria currently works with four different systems across its 77 heath services.

The Australian government will invest $345 million for on-site pharmacists and pharmacy services at government-funded residential aged care facilities to help improve medication management in the sector.
The funding is being touted as a complement to ongoing improvements in the digital capabilities of RACFs to support medication management services and ensure safe use of medications.
UK’s first digital health training program, US doctors use audio-only telehealth, NHS access to GP records, managing COVID at home with telehealth, fake EU Digital COVID certificates, security and remote patient monitoring, why FHIR is utterly powerful, Northern Ireland’s digital health strategy, Scotland’s medical interoperability gateway
UK’s first digital health training programme launches for NHS frontline staff
Medical Device Network ~ Kezia Parkins ~ 24/03/2022
Developed by ORCHA and the NHS, the Digital Health Academy will be available to frontline staff to improve uptake of digital health tools.

This week started off with the interesting news that private health insurer Medibank had invested $10 million in telehealth start-up Medinet. Telehealth start-ups are of course a dime a dozen, promising to revolutionise this and disrupt that, but that’s been the case for the last 10 years or so for those in the business.
We’ve been reporting on telehealth for 15 years and remember the big uptake beginning in 2010-2012, along with health insurer interest in telehealth platforms. For instance, HCF took an early stake in long-standing platform GP2U, which recently sold to UK-based telehealth provider Doctor Care Anywhere for $11m.

South Australia's new health minister Chris Picton was sworn in yesterday, following last week’s election win for Labor.
The 39-year-old Mr Picton was chief of staff to John Hill, a former SA health minister and MHA for the same seat of Kaurna. He also had a stint as staffer to former federal health minister Nicola Roxon.

The private hospital sector claims it has been “blindsided” by new requirements under the federal government’s Critical Infrastructure Protection Bill, which they say may lead to them closing down intensive care units due to cost.
The bill is designed to ensure Australia’s critical infrastructure can defend itself against cyber attacks. Both public and private hospitals with ICUs are considered one of those critical industries.
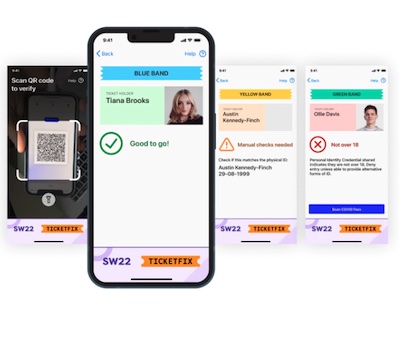
New Zealand will phase out the requirement to use vaccine passes as part of its COVID-19 protection framework (CPF) from April 4, and is also dropping the need to scan in QR codes when entering businesses.
New Zealand Prime Minister Jacinda Ardern has announced that as the country moves into a different phase of its CPF or traffic light system, certain mandates brought in during the Delta wave are no longer necessary with Omicron.

Sydney Local Health District's Royal Prince Alfred Hospital will trial a new eReferral system for fertility, gynaecology and maternity services as part of eHealth NSW’s Engage Outpatients pilot from late next month, along with a new fax coversheet which enables digitisation of faxed referrals for GPs who are not eReferral-enabled.
Sydney LHD has been using HealthLink’s SmartForms for eReferrals to certain ambulatory care services at Concord and RPA hospitals since last year, but Engage Outpatients will involve maternity services at RPA in late April and at Canterbury Hospital later in the year as part of the pilot.

Foxo has launched a new Guest Chat function in its clinical workflow and communication platform that allows clinicians to embed a simple URL in clinical documents, SMS or emails that forms a one-click secure communication gateway.
The module has been designed to overcome the problem of long call queues and abandoned calls to streamline inbound communication between Foxo-enabled organisations and their referrers and extended clinical networks.
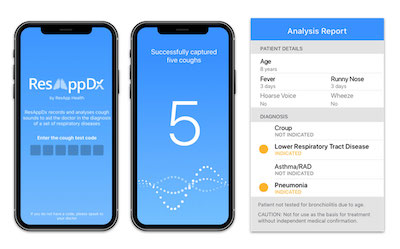
ASX-listed respiratory app technology developer ResApp is in the early stages of planning a randomised control trial of its new app-based diagnostic screening tool for COVID-19, following early results showing it had high sensitivity and good specificity.
The early clinical results showed it has potential use as a mass screening test prior to rapid antigen or polymerase chain reaction testing to rule out COVID-19.

The Australian government plans to set up a new Genomics Australia agency to accelerate the translation of genomic technologies into clinical practice and public health services.
The agency, which will be a legislated corporate Commonwealth entity under the health portfolio from January 1 2024, was welcomed by the Australasian Institute of Digital Health (AIDH) and the Industry Genomics Network Alliance (InGeNA).

InterSystems has released of a new platform-as-a-service (PaaS) with HealthShare Health Connect Cloud, promising to streamline interoperability and data integration between clinical systems and applications.
InterSystems says Health Connect Cloud enables healthcare organisations to take advantage of the security benefits of the cloud while providing scalability and high availability, and minimising the time and effort required to deploy and operate the system.

Faxed requests for cervical screening histories to the National Cancer Screening Register (NCSR) have dropped by 94 per cent in one year following the introduction of a provider portal and integration with practice management systems.
The NCSR is reporting big uptake of online alternatives, including the provider portal rolled out to allow GPs and practice staff to access real-time patient data via PRODA in October 2020.

Private health insurer Medibank has invested $10 million in emerging online healthcare platform Medinet, which facilitates GP consults by video, audio and chat.
Launched in 2019, Medinet claims an average of 10,000 people are using it each day, and is among the top five most downloaded healthcare apps in Australia.


Microsoft adds virtual care to Teams, can a hospital run safely without an EMR, machine learning tool for COVID death risk, telehealth a barrier to showing empathy to patients, first health organisation achieves triple HIMSS level 7 status, US standard for voluntary national patient credential
Microsoft Teams adds new virtual care features
mHealth Intelligence ~ Anuja Vaidya ~ 16/03/2022
The features, which include enabling organizations to collect patient triage information, and access analytics, aim to enhance the virtual visit experience within Teams.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.