Telstra has announced a loss of $38 million in an overall $77m impairment reduction for its health business and a dilution of its ownership of online booking service Health Engine, but says it is looking at a long-term strategy for the division and expects it to become profitable.
Announcing its end-of-financial year results last week, the company said Telstra Health was now the largest health software and solutions vendor in Australia and had over 1000 people on staff.

Primary Health Care is gearing up for the roll out of MedicalDirector's Helix cloud-based practice management system to its medical centres later in the year, along with the new Visage radiology information system from Pro Medicus that it plans to roll out to Healthcare Imaging Services, the company's diagnostic imaging division.
Primary also plans to upgrade its pathology laboratory information system and its underlying infrastructure, and to begin the development of mobile applications and portals for its new Health & Co mixed billing medical centres business.

Fremantle Hospital will join WA's flagship Fiona Stanley and 17 other hospitals in the state in using Core Medical Solutions' BOSSnet electronic medical record, with plans to roll out BOSSnet's electronic forms and scanning modules later this year.
Fremantle and Fiona Stanley are both part of the South Metropolitan Health Service and patient transfers between the two hospitals are a daily occurrence.
Adelaide-based Core Medical Solutions (CMS), which was acquired by US EMR giant Allscripts in December last year, has now rolled out BOSSnet to over 100 hospitals, including eight Epworth Healthcare sites in Melbourne and Geelong, Western Health, Barwon Health, Ballarat Health Services and it is shortly to go live at the Grampians Rural Health Alliance.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending August 20:
Why one practice ditched EHR in favor of paper records
FierceHealthcare ~ Joanne Finnegan ~ 14/08/2017
The Illinois Pain Institute has done what many physicians only dream about doing. The practice, which has multiple locations in four Illinois counties, just ditched its electronic health record (EHR) and went back to paper records.
New York hospitals say telehealth helped slash ER wait times, enhance care
Healthcare IT News ~ Bill Siwicki ~ 17/08/2017
While the average emergency room wait times for low-acuity patients were up to two-and-a-half hours at NewYork-Presbyterian and Weill Cornell Medical Center, the provider’s Telehealth Express Care service can get patients in and out in 35 minutes.

It was no surprise that the most popular story this week on Pulse+IT was our report on a workshop on secure messaging held at the HIC conference in Brisbane, where it was revealed that the National Authentication Service for Health (NASH) needed a major overhaul if it was ever going to be of any use to anyone.
Developing a useable authentication system has been a bottomless pit from which little has emerged in the decade or so that we've been covering it. As we wrote back in 2010, NASH has been an integral part of the eHealth agenda since NEHTA's inception in 2005, but where once outsourcing sounded good it quickly turned terminal, and even though the Department of Human Services came to the rescue in the PCEHR days, NASH has caused trouble ever since.

A project to build a database of the various clinical IT implementations and technologies used in Australian hospitals has kicked off in the hope that the information can be shared for the benefit of the health IT community.
The brainchild of Checkley Group managing director Bruce Pedersen, the project is still in its early stages but the long-term idea is to gather data on implementations and different technologies used to then be able to measure their worth in terms of workflow improvements, clinical documentation support and device integration.

Not-for-profit digital health accelerator ANDHealth has moved into the specialised working facilities of Agnes Health in East Melbourne, aiming to make it the precinct a hub for mid-stage digital health technology companies and entrepreneurs.
ANDHealth is a new national digital health initiative partially funded by MTPConnect, a federal government industry growth centre program, with funds matched by commercial partners including Novartis, the Murdoch Childrens' Research Institute (MCRI), Curve Tomorrow and telehealth provider GP2U.

Hunter New England Health is set to roll out the Patientrack patient deterioration early warning and alerting system at Maitland Hospital near Newcastle in the next few months before it is progressively rolled out to the rest of the LHD.
Patientrack was devised by a New Zealand-trained intensive care specialist based in the UK and has been deployed in a number of NHS hospitals as well as four district health boards in New Zealand.

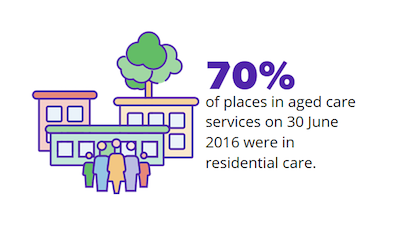
The Australian Institute of Health and Welfare (AIHW) went live yesterday with a new website called GEN that provides access to aged care data held in the National Aged Care Data Clearinghouse.
Designed to cater to all levels of users from school students to aged care residents, researchers and data modellers, the site contains data on capacity and activity in the aged care system, focusing on people, their care assessments and the services they use.
Brisbane's Mater Group has finished the deployment of the OnBase by Hyland enterprise information platform at its seven hospitals and is now planning to ready itself for an electronic medical record by 2020 as part of its overall digital strategy.
Mater Group first went live with OnBase at Mater Private Hospital Redland in October 2015 for its scanning and document capture functionality, with the digital record viewed through the Verdi clinical portal, which has been in use at the Mater since 2007.

Adelaide's Getz Clinical has launched a surgical module that enables surgeons to record and document surgical procedures, annotate data from imaging devices and produce surgical reports as part of its wider suite of perioperative electronic medical record solutions.
The module has been built in conjunction with surgeons from Australia, Canada and the Philippines to allow them to improve the accuracy of their records and to expedite data entry.

Secure messaging vendors will have the ability to issue authentication certificates on the spot and use their own identifiers as an interim measure while work continues on making messaging systems interoperable, with a project also underway on a FHIR-based directory standard that will allow rival vendors to query each other's address books.
Variously describing the National Authentication Service for Health (NASH) and the Healthcare Identifiers (HI) Service as “failures”, “unwieldy” and “unsuccessful”, messaging vendors told the Health Informatics Conference (HIC) in Brisbane last week that an agreement to give vendors more control over the interoperability agenda was soon to be signed.

Melbourne-based Windana Drug and Alcohol Recovery Inc is about to start a pilot program aimed at measuring the outcomes of its work, rather than the more common outputs, and is currently looking for an IT solution that can help the organisation collect and analyse data.
Windana, which offers adult withdrawal and recovery services from its headquarters in St Kilda along with a youth service in Dandenong and a long-term residential facility in rural Maryknoll, receives funding from the Victorian Department of Health and Human Services as well as donations and philanthropic support for the 2000 or so people it helps each year.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending August 13:
Microsoft unveils open source Coco blockchain framework for healthcare
Healthcare IT News ~ Tom Sullivan ~ 10/08/2017
Hospitals can use the tech to create blockchain networks with governance, security and other transactional capabilities, the company says.
Allscripts scoops up NantHealth provider, patient engagement business
Healthcare IT News ~ Bernie Monegain ~ 10/08/2017
The EHR maker, fresh off a major deal with McKesson, exchanged its ownership interest in NantHealth.

Pulse+IT spent a couple of days at the annual HIC conference this week, basking in the glorious sunshine that BrisVegas likes to shower on its lucky inhabitants even in winter. It was nice to see all of the big EMR vendors there and they were all very nice to us, even those whose reputations we were busy tarnishing with some of our reporting in the last few weeks.
Cerner was in the news through a combination of our stories on the disquiet in Queensland over the planned new anaesthesia module and there was also a nice anecdote that ADHA CEO Tim Kelsey told at HIC about how he unexpectedly ended up in hospital in Sydney recently and was able to observe first-hand the frustration and rage felt by some clinicians when dealing with electronic systems.

NZ's Ministry of Health will release a request for information next week looking for cost estimates and potential options for the national electronic health record (EHR) project.
As Pulse+IT reported last month, the government has asked the Ministry for further analysis on the costs and benefits of a national system following a review of the indicative business case (IBC) in early July. The Ministry is due to report back to Cabinet in December.

A senior ICU specialist at Adelaide's Repatriation General Hospital has rejected claims that South Australia's Enterprise Patient Administration System (EPAS) is dangerous following the release of an AMA survey of doctors' views on the system, which showed there are still concerns over its interface and the time it takes away from patient care.
Some users also have significant concerns over its safety, with the AMA's South Australian branch president William Tam saying doctors had reported many near-misses and that it could potentially be dangerous when it is introduced to the new Royal Adelaide Hospital (nRAH), which opens after much delay next month.
However, Repat General intensive care specialist and chair of the EPAS clinical advisory committee Santosh Verghese said the system had been used at his hospital and others, including the most recent roll-out at The Queen Elizabeth Hospital (TQEH), and there was no evidence for the danger claim.

The Australian Digital Health Agency (ADHA) has come to an agreement with six community pharmacy software vendors to assist them to connect to the My Health Record system, joining market leader Fred IT and Simple Retail, which were the two original members of the NEHTA pharmacy software vendors panel and have been connected to the system since about 2013.
The additions include the Minfos dispensing system, which is owned by EBOS Healthcare and is widely used in Terry White and Chemmart outlets, along with Dispense Works, owned by Queensland vendor POS Works and which launched in 2015, and smaller players Mountaintop Dispense, RxOne, ScriptPro Dispense and Z Dispense.
The vendors are being subsidised for their integration work at variable rates of between $130,000 and $250,000.

Former Royal Brisbane and Women's Hospital CEO and NHS England chief clinical information officer Keith McNeil is returning to Brisbane from the UK to take up the newly created role of assistant deputy director general and chief medical information officer (CMIO) with Queensland Health.
Professor McNeil, a lung transplant specialist and respiratory physician who once served in the Australian Special Forces as a weapons expert, was also CEO of Addenbrooke’s Hospital and Cambridge University Hospital Foundation Trust when that organisation went through a much-criticised implementation of an Epic electronic medical record that has since been held up as one of the best in the UK.

The Australian Digital Health Agency (ADHA) intends to publish a draft plan for interoperability standards for healthcare providers by the end of this financial year, which CEO Tim Kelsey described as a 'licence to operate' that organisations in both the public and private sectors will need to adopt.
ADHA released the long-awaited national digital health strategy last Friday following its endorsement by the COAG Health Council. The strategy involves seven priorities, one of which is the development of a set of agreed standards for interoperability and a roadmap for implementation that will see regions showcasing comprehensive interoperability across health service provision by 2022.

Precedence Health Care CEO Michael Georgeff was awarded Australia's top prize for excellence in primary care informatics at the Health Informatics Conference (HIC) in Brisbane yesterday, accepting an award named in honour of the much-admired health informatician – and Professor Georgeff's colleague at Precedence – the late Jon Hilton.
Another long-serving member of the health informatics community, David Rowlands, was made an honorary life member of the Health Informatics Society of Australia (HISA) at its annual awards, while NSW Health's chief clinical information officer John Lambert was elected to the society's board.

Auckland-headquartered Orion Health has won a contract with the Victorian Department of Health and Human Services (DHHS) to roll out its Rhapsody integration engine as part of a five-year program to replace the JCAPS-based legacy system across the department and 15 public health agencies.
Orion Health completed a similar implementation for Ballarat Health Services in 2013 and is also at the start of a large implementation of Rhapsody for Queensland Health.

The Victorian government has decided to build its own real-time prescription monitoring (RTPM) system as part of its $29.5 million project, rejecting the national electronic reporting and recording of controlled drugs (ERRCD) system that the federal government plans to implement.
Victorian Health Minister Jill Hennessy introduced legislation to state parliament today to smooth the way for the system to be rolled out from next year. Victoria has chosen to apply real-time monitoring to Schedule 4 drugs, including all benzodiazepines, as well as Schedule 8 controlled drugs such as opioids.

Adelaide-based Getz Clinical has launched a new analytics module to complement its perioperative electronic medical record system in advance of plans for the release of a new surgical module in the next few weeks.
Getz Clinical, part of the international Getz Group, includes Queensland Health, SA Health and Forte Health in NZ as clients. The new Analytics+ tool is aimed at both clinical and non-clinical users to allow them to capture, process, analyse and distribute reports and dashboards.

Former PCEHR review chairman and start-up adviser to the Australian Digital Health Agency Richard Royle is leading a move to develop a new professional college for digital health executives, aimed at providing continuous education and career paths for the emerging profession.
Mr Royle told the Health Informatics Conference (HIC) in Brisbane yesterday that the plan was to cover both Australia and New Zealand, with the college tentatively named the Digital Health Executives Network of Australasia.

The nursing and digital health peak bodies have released a position statement on the role of nurses in the adoption of digital health technologies, warning that the 'build it and they will come’ view without clinician involvement has not been successful and the health sector's largest profession needs a seat at the digital health table.
Released at the Health Informatics Conference (HIC) in Brisbane on Sunday, the positions statement advocates for the instrumental role of nurses in digitally transforming healthcare and makes a call to optimise the use of information technology to enable better patient care.

Queensland Health has defended the functionality of the anaesthesia solution it plans to roll out as part of its digital hospital program, despite criticism from a group of senior anaesthetists who say it doesn't have the functionality of the existing system.
Pulse+IT has heard from a number of doctors who have inspected the software, Cerner's anaesthetic solution (SAA), that it only has about 80 per cent of the capability of the existing solution, WinChart, which is known in Queensland as Automated Anaesthetic Record Keeping (AARK).

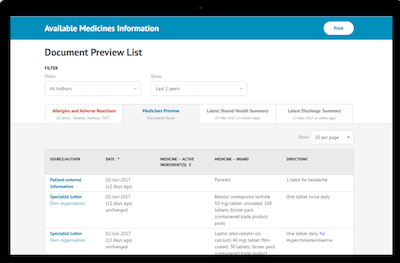
A literature review and environmental scan are currently underway to lay the groundwork for a two-year project looking at how the My Health Record can be used in hospital emergency departments to allow ED clinicians to access patient data such as medications and allergies in real time.
The project is one of six 'test beds' outlined in the National Digital Health Strategy and will involve EDs in the Nepean Blue Mountains and Northern Queensland Primary Health Networks (PHNs), where the vast bulk of the local population has a My Health Record, and will eventually lead to the development of a model that other hospitals can use to introduced the record to ED workflow.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending August 6:
Thousands of patients may need to have tests redone over IT flaw
Irish Times ~ Paul Cullen ~ 03/08/2017
It has been discovered that when images are archived, the “less than” symbol, “
How Jared Kushner helped the VA pick Cerner... quickly
Healthcare IT News ~ Bill Siwicki ~ 03/08/2017
Many people in the government and healthcare sectors were surprised at how quickly the VA made its choice and the fact that it did so without the usual request for information and request for proposal procedures that are common in large-scale IT acquisitions.

It didn't come as much of a surprise to learn late on Friday that the Council of Australian Governments (COAG) Health Council had given the go-ahead to the new national digital health strategy. After all, it was revealed just recently that the state and territory health departments were all pretty keen on it and had recommended that everyone at COAG say aye as well.
What has come as a surprise is that the strategy is actually pretty good. We were dreading the usual high falutin' but meaningless verbiage that usually infests these documents but while the strategy is a bit too long, it is at the same time succinct, and more importantly it is written in plain English so even nincompoops like us can understand it.

The COAG Health Council has given the green light to the National Digital Health Strategy, which aims to ensure health information is available to patients and providers whenever and wherever it is needed by 2022.
Written by the Australian Digital Health Agency (ADHA) and supported by all of the state and territory health departments, the strategy outlines seven priority areas with defined outcomes, along with a series of six 'test beds' to trial digital solutions to pressing health issues.
Top of the list of priorities is access to information when it is needed through systems such as the My Health Record; secure information exchange for all healthcare providers and consumers through secure messaging; systems interoperability through agreed standards; new models of care enabled by eHealth such as healthcare homes; a digitally confident and capable healthcare workforce; and a thriving digital health applications and software industry.

Some of the most senior anaesthetists in Queensland are set to go public with serious concerns about the roll-out of a new anaesthetics module as part of the state's integrated electronic medical record (ieMR), saying the new solution does not have the capability of the existing WinChart system, implemented a number of years ago for the state's Automated Anaesthetic Record Keeping (AARK) program.
Queensland Health is currently trialling the new module – the SurgiNet anaesthesia application from Cerner – through the Medications, Anaesthetics and Research Support (MARS) program being piloted at the country's first major hospital to go digital, Brisbane's Princess Alexandra Hospital (PAH).
It is set to then be rolled out to other hospitals using the advanced ieMR including Cairns and Townsville. Pulse+IT understands that senior anaesthetists from Mackay, Logan, Bundaberg, QEII and Toowoomba hospitals have been told that they must implement the solution, despite a widespread belief that it is inferior to WinChart and other perioperative solutions on the market.

Royal Melbourne Hospital and its partner facilities in the Parkville precinct are still working towards a long-term shared electronic medical record after an ambitious business case for a full EMR, strongly rumoured to be supplied by Epic, failed to receive funding in this year's state budget.
The new plan involves a re-scope of the original proposal with some functionality to be introduced in the early stages, including a solution to replace the Symphony emergency department system, which vendor EMIS Health will no longer support after December.

Western Victoria Primary Health Network (PHN) will lead a consortium including all Victorian PHNs and NPS MedicineWise to develop and deliver the training and education package for doctors and pharmacists that makes up a central plank in the state's real time prescription monitoring system.
The Victorian government allocated just over a million dollars for education and training as part of its overall $29.5 million RTPM package, which it announced last week would include Schedule 4 medicines implicated in misuse such as benzodiazepines and Stilnox as well as Schedule 8 controlled drugs such as opioids, Xanax and Ritalin.

The HealthOne shared care records program has gone live in the last of the five district health boards on New Zealand's South Island, representing the final link in the chain that will allow health professionals in both primary and secondary care to view a patient's health information.
HealthOne was first developed through a partnership between Canterbury DHB, primary care network Pegasus Health and clinical software vendor Orion Health in the aftermath of the 2011 earthquakes that devastated Christchurch. It has since been rolled out to South Canterbury, Southern and West Coast DHBs and is now accessed more than 3000 times a day.

Online appointment booking and directory service HealthEngine has appointed former Citibank IT director Mark Hammond as its new head of technology, engineering and data security as part of an employee growth phase powered by a recent capital raising.
The Perth-based firm, which counts Telstra and Seven West Media as early investors, has also opened new offices in Sydney and Melbourne and appointed a former LinkedIn Australia staffer, Mark Dick, as head of sales.

Blood availability information from NSW Health Pathology has recently been added to the NSW Trauma app to enable pre-hospital teams to rapidly access additional blood products in critical situations.
The app, which recently won a public sector and government merit award at the NSW iAwards, is also being used by Queensland Health and the New Zealand Major Trauma National Clinical Network, where it has been mapped to trauma facilities across NZ.
It features a critical care geospatial function which has the ability to locate blood products for use in pre-hospital or inter-hospital retrieval, allowing clinicians to provide appropriate blood transfusions to critically injured patients, something that previously has been only available in hospitals.

Perth-based home infusion service chemo@home is rolling out EpiSoft's cloud-based chemotherapy management platform Cancer CareZone to allow its nurses to access clinical data on their mobile devices.
Sydney-based EpiSoft first launched CareZone in 2014 and it was later implemented at the Sydney Adventist Hospital, and has now been rolled out to five states. EpiSoft also developed the web-based eAdmissions module that is in use in over 60 hospitals.

MIMS Australia has partnered with Fred IT to integrate its internet-based medicines information application eMIMSCloud with Fred's cloud dispensing platform Fred NXT.
Going live tomorrow, the integration will see Fred NXT users able to add eMIMSCloud to the app bar in Fred NXT, allowing pharmacists to click on the eMIMSCloud tile and go straight to the relevant information about a medicine as they dispense.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending July 30:
People want to share their health data with Google, report reveals
Digital Health News ~ Shireen Khalil ~ 26/07/2017
The highly anticipated report, Internet Trends 2017, reveals that people are willing to share their health data with leading tech brands such as Google, proving their position in the digital health market.
Sutter Health to help small hospitals use virtual PCs
Health Data Management ~ Joseph Goedert ~ 26/07/2017
Sutter Health is in the early stages of offering smaller hospitals a virtual personal computer infrastructure that will enabling an organization’s users to move from one machine to another throughout a facility, or access information from a mobile device of their choice, such as a tablet.

Pulse+IT was indulging in a session of Olympic-class eye rolling on Friday after we received a bunch of tweets telling us that Greg Hunt was boasting his government was going to solve the long-term problem of accidental prescription drug overdoses by funding the roll-out of a national real-time prescription monitoring scheme to the tune of $16 million.
We've covered this topic at length for many years now and were there the last time this scheme was announced, which was back in 2012 and by a different health minister in a different government and costing $8m at the time. (This of course followed $5m being allocated two years before that, in the Fifth Community Pharmacy Agreement.) It's the same old story though: here's a problem we know about, here's one way we can help solve it, let's do very little for five years and then – ta-da! – here's $16 million and a nice press release. All sorted.

The Victorian government will include benzodiazepines and so-called 'Z class' sleeping pills in its $30 million real-time prescription monitoring system expected to be rolled out next year, with codeine to be added at a later stage.
On a day that the federal government announced it would chip in $16 million to see the long-delayed Electronic Reporting and Recording of Controlled Drugs (ERRCD) finally rolled out nationally, Victorian Health Minister Jill Hennessy announced that her state would take a harder line on high-risk prescription drugs, including some Schedule 4 drugs in the scheme and making it mandatory for doctors and pharmacists.
The national system has been designed only to monitor Schedule 8 drugs of addiction such as opioids, despite calls for certain S4 drugs and codeine, which is shortly to be rescheduled to S4 prescription-only from S3 pharmacy-only, to also be monitored.

The federal government has agreed to invest over $16 million to realise the belated roll-out of a real-time prescription monitoring (RTPM) scheme, which will be based on the Electronic Reporting and Recording of Controlled Drugs (ERRCD) system first announced by the previous government in 2012.
After years of pressure to introduce the system from medical and pharmacy groups, the medical software industry, patient advocacy groups and several state coroners, the government announced today that it would move to introduce the system on a national scale to alert pharmacists and doctors if patients received multiple supplies of prescription-only medicines.

Just over five million Australians are now registered for the My Health Record, just on five years after the system went live.
Of the 5,031,144 individual people registered, which represents one in every five Australian, 54 per cent are female and 46 per cent male.

The Northern Territory has become the second jurisdiction to begin uploading pathology reports from its public health facilities to the national My Health Record (MyHR), having uploaded over 3400 since the functionality went live late last month.
NT clinicians can also still view results from private labs through the NT My eHealth Record, which is being kept active for the time being and is available in a combined view with the national system through the eHealthNT Clinical Portal (NTCP).
Sydney-based health informatics firm Ocean Health Systems and telemedicine specialist Livecare have joined forces to offer a combined package aimed at healthcare homes and integrated care initiatives that embeds telehealth capabilities within a shared care plan to easily connect patients to the care team.
The new approach will allow any member of the care team to communicate directly with patients about their care plan remotely, without requiring face-to-face meetings, and care team members will also be able to communicate securely with each other and hold case conferences with up to 14 carers and the patient themselves.

Western Victoria Primary Health Network (WVPHN) is collaborating with patient self-management specialist Healthily to roll out Healthily's GoShare patient education platform to 800 GPs and pharmacists.
Healthily allows health professionals to send tailored, evidence-based information to patients in a variety of formats such as video, animation, text and apps as a way to back up face-to-face or telehealth consultations with extra information, particularly in relation to the self-management of chronic conditions.

The New Zealand Ministry of Health (MOH) has revealed a plan for the next 12 months in the development of the country's national electronic health record (EHR) following a request from a cabinet committee for more detail on the costs and benefits of the proposed system.
As Pulse+IT reported recently, the Cabinet Committee on State Sector Reform and Expenditure Control (SEC) – which is chaired by Minister for Finance Steven Joyce and considers all large investment projects – earlier this month requested more detail on the costs, benefits and risks of the EHR, to be submitted as an addendum to the indicative business case (IBC) prepared by Accenture.

WA-based ISA Healthcare Solutions is in the middle of an implementation planning study (IPS) to prepare for the roll-out of its MMEx web-based clinical information system for the much-anticipated Regional eHealth Project for rural and remote communities in far north Queensland.
The project will see an integrated point-of-care clinical record rolled out covering primary, community and some acute care settings in the region as part of an overall $35 million project, a joint eHealth initiative between the Cairns and Hinterland Hospital and Health Service (HHS) and Torres and Cape HHS.
It will be integrated with existing Queensland Health administrative and clinical systems such as Active Directory, the pathology system Auslab and The Viewer, with plans for an interface between MMEx and the state's Cerner-based ieMR, along with the national My Health Record.

The Queensland government will require pharmacists to report when they dispense Schedule 8 (S8) drugs of addiction on a weekly rather than monthly basis but will only begin developing a business case for implementing real-time reporting later this year, despite technology enabling real-time prescription monitoring (RTPM) being made available five years ago.
Queensland Health Minister Cameron Dick said his department would consult with pharmacists and doctors on the move, which comes as Australian Bureau of Statistics data show that prescription painkillers have overtaken illicit sources as the underlying cause in most accidental opioid overdose deaths.

A Wollongong Hospital nurse has developed an informative and easy to use smartphone app aimed at reducing patient-related day-of-surgery cancellations that he hopes can be simply and cheaply adopted by every surgical hospital in the country.
Called My Surgery Journey, the app is accompanied by a 24-page printed magazine that includes all of the information patients need when preparing for elective surgery, including directions to the hospital, advice on fasting and medications such as aspirin that can effect surgical procedures, and what patients should do if they are feeling unwell before surgery.
Developed at a bargain price of $22,000, the result of a Illawarra Shoalhaven Local Health District (ISLHD) Illumination Innovation grant, clinical nurse consultant James Brinton hopes that other hospitals will now adopt the app and add their local details or extra functionality to it, improving the app by collaboration over time.

New review highly critical of NHS Digital’s capabilities
Digital Health News ~ Laura Stevens ~ 19/07/2017
A critical internal review of NHS Digital has found the organisation relies on out of date technology, has skill shortages in multiple areas and its data services are operating below expectations.
Workflow integration is a bigger problem than interoperability
MobiHealthNews ~ Jonah Comstock ~ 20/07/2017
Dworkin says that workflow integration is actually a bigger problem then that favorite complaint of the health IT space, interoperability.

In what is an unusually quiet period for the normally super-active eHealth sector, our top story this week turned out to be the fortnight-old news that the draft of the long-promised national digital health strategy would be on the agenda of the COAG Health Council when it meets next month.
We first heard about this on July 4, although to be honest it's not a secret. Having been delayed repeatedly since 2013 and rewritten a couple of times, the strategy was next scheduled for November 2016 but was delayed yet again until the newly appointed Australian Digital Health Agency CEO could put his mark on it.

The Victorian government has announced the four pilot sites for its pharmacist chronic disease management trial, which will see pharmacists providing regular monitoring, dose refinement and earlier intervention for patients with a GP care plan.
Targeting people with chronic conditions such as asthma or high blood pressure, the trial will allow patients to visit their local pharmacy when monitoring and managing their chronic illnesses.

A look at the factors impeding interoperability between medical software systems and a discussion on the application of sound health cybersecurity practices are two of a series of specialist workshops scheduled for HISA's Health Informatics Conference (HIC), being held in Brisbane in August.
Medical software industry stalwarts Tom Bowden from HealthLink, Medical-Objects' Andrew McIntyre, Best Practice's Frank Pyefinch and former HealthConnex MD Peter Young, who is advising the Australian Digital Health Agency (ADHA) on its secure messaging program, will speak at the secure messaging interoperability masterclass, chaired by Medical Software Industry Association (MSIA) president and Extensia CEO Emma Hossack.

Consumers are happy to have medical data transmitted from medical devices such as blood sugar sensors to their clinicians but are far more reluctant to accede to other remote monitoring such as giving employers or insurers access to fitness tracker data, a new survey has found.
The findings from the 2017 Unisys Security Index show that overall, consumers need a compelling reason to allow connected devices to gather and transmit their personal data. Unisys markets security and medical device management solutions to the healthcare industry, among others.

A draft of the much-delayed Australian national digital health strategy is expected to be presented to state and territory health ministers at the next COAG Health Council meeting, scheduled for some time next month.
A refresh of the original 2008 strategy was completed in 2013 but has never been released publicly, with a new draft written in 2015, with excerpts published by Pulse+IT in 2016.

CSIRO has gone live with a new $4 million supercomputer from Dell EMC, aimed at expanding the organisation's capability in deep learning and artificial intelligence.
Nicknamed 'Bracewell' after Australian radio astronomer and engineer Ronald Bracewell, whose work led to advances in medical imaging, the system will provide capabilities in areas such as virtual screening for therapeutic treatments and machine learning for image recognition, as well as modelling new material structures.

WA Primary Health Alliance (WAPHA) and workforce agency Rural Health West have commissioned a research study to identify and overcome barriers to wider adoption of digital health technologies such as telehealth in general practice in rural and remote Western Australia.
The Country WA Digital Readiness project will use the research skills of the Australia and New Zealand Cooperative Research Centre for Spatial Information (CRCSI) to look at the size, location and connectivity of general practices in country WA to work out if geography could be hindering the uptake of digital technologies.

Digital health platform Healthshare has added the Australian Health Service Alliance (AHSA) to its specialist cost transparency scheme, which allows GPs to use its specialist directory to quickly find whether a medical specialist participates in a fund’s no gap or known gap scheme through the GP's clinical software.
AHSA represents 27 different private health insurance funds and joins market leaders HCF and Medibank in listing gap cover participation in Healthshare's directory, which now covers most of the 37 funds in Australia.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending July 16:
Threats to information security: public health implications
New England Journal of Medicine ~ William J. Gordon ~ 12/07/2017
In health care, information security has classically been regarded as an administrative nuisance, a regulatory hurdle, or a simple privacy matter.
Patient access to medical records continues to be challenging
Health Data Management ~ Greg Slabodkin ~ 13/07/2017
Although electronic health records are widely used by providers, patients continue to face challenges in accessing their healthcare information, according to a new study funded by the Office of the National Coordinator for Health IT.

One of the most popular stories this week on Pulse+IT was our article on Queensland's move to allow GPs to take a look at their patient's hospital medical record through a new portal that links to Queensland Health's The Viewer, the web-based application that lets QH clinicians see patient data from different clinical systems and different hospitals throughout the state.
The Queensland government had to write new legislation last year to get the system up and running, and from what we hear, it is going to be a very popular move. There are strict privacy and registration procedures that GPs have to go through, including lots of hoops to prove their identity before they are allowed to register, but in the wake of last week's revelation that it may be the HPOS system at fault for the Medicare number leak, that's probably not a bad thing.

The New Zealand government has asked its health ministry for further analysis on the costs and benefits of the proposed national electronic health record (EHR) before giving the project the go-ahead, with an addendum to the current indicative business case expected to be considered for approval by Cabinet in December.
In the meantime, work will begin next month on the promised national digital health strategy, guided by the 'living vision for health technology' that is set to be published shortly. Deputy chief technology and digital services officer – eHealth Darren Douglass told Pulse+IT that the vision had been endorsed by the Digital Advisory Board in June and is currently being prepared for publication.

The cancer multidisciplinary meeting (MDM) system developed in-house by Southern District Health Board in 2013 is set to roll out to the rest of the South Island progressively from the end of this month, accessible to teams through the island-wide Health Connect South clinical portal.
The single, shared MDM system allows a range of specialists to case conference and share care plans and treatment options for individual patients electronically, overcoming timeliness and care coordination barriers caused by paper correspondence and discrete databases and spreadsheets.

Primary health organisations (PHOs) that were holding out on agreeing to general practices having to pay a $2 fee to transfer medical records to a patient's new practice have come to an agreement with GP2GP service provider Patients First, giving the go-ahead to an annual fee per patient instead.
GP2GP, developed by the practice management software vendors and Patients First with the support of secure messaging provider HealthLink, has seen over a million messages transferred since it was first developed in 2011.

Former home and community care provider HHL Group manager Mark Leggett has been appointed as general manager of the South Island Alliance, replacing Jan Barber, who was in the role for six years.
A collaboration of the South Island’s five DHBs, the SI Alliance oversees a number of functions including information services and is in charge of the implementation of the single South Island-wide patient management system being built by Orion Health, known as SI PICS.

Queensland GPs can now access their patients' hospital medical records with the launch of a new health provider portal (HPP) that links securely to Queensland Health's The Viewer web-based clinical application.
Part of the state's $361 million specialist outpatients strategy, the idea is to provide GPs with read-only access to a summary of diagnoses, pathology and diagnostic imaging results, and medications prescribed and administered while the patient is being treated in hospital.

Update: Trials to demonstrate an interoperable system of secure messaging between healthcare providers have already got underway despite no official announcement about which organisations have won funding to run them.
As Pulse+IT reported last week, one consortium involves the four leading secure messaging vendors – HealthLink, Medical-Objects, Global Health and Argus, which is owned by Telstra Health – along with GP desktop software vendor Best Practice and medical specialist software market leader Genie Solutions.

The federal government has announced the winning bidders in the Dementia and Aged Care Services (DACS) research and innovation funding round, which will see 42 projects funded for the next two years to strengthen the capacity of the aged care sector to respond to consumer-directed care and the challenges of dementia.
The projects were chosen from six priority areas, including virtual care, adaptive and assistive technologies, and the development of smart home devices and platforms to enable people to live safely in their homes for longer.

Melbourne-based start-up Health Delivered has received funding from digital commercialisation firm Trajan Scientific and Medical to help it launch its cloud-based dietary management platform, which is due to go into beta testing next month.
The platform will initially be aimed at dietitians but the plan is to extend it to aged and community care as well as hospitals and sports nutrition, with the ability to generate meal plans during a consultation and take in data from wearables and remote medical devices.

The Gold Coast Health and Griffith University team that recently won Queensland's top eHealth award for developing an automated system to manage elective surgery waiting lists is now turning its attention to adapting the system for wider use, including theatre management and emergency department patient flow.
The MIS team, led by Centre for Health Innovation executive director Martin Connor and project director Steve Gough, has developed an automated, web-based system that enables surgical teams to see their waiting list every morning, updated almost in real time, along with an application that automatically identifies which patients need to be seen as a priority.

ASX-listed eHealth solutions vendor Global Health has officially released its LifeCard patient portal, having tested it out in five sites using the company's patient administration and electronic medical record systems.
The portal is expected to enable hospitals and day surgeries to reduce cancellations and save on administration costs, with one hospital estimating online pre-admission saved around 15 minutes per patient.

The Centre for Public Health Research (CPHR) at Massey University's Wellington campus has launched New Zealand's first master's degree in analytics specialising in health, aiming to fill a growing need for people able to analyse, interpret and disseminate health data.
With employment in the ICT management, health services management and health analytics fields projected to grow by up to 5.3 per cent in NZ and 7.2 per cent in Australia, the CPHR's associate director Barry Borman said New Zealand needed to generate homegrown capability to fill a shortage.

The federal government has commissioned a review into the Department of Human Services' Health Professional Online Services (HPOS) system following the revelation last week that Medicare numbers have been offered for sale on the internet.
HPOS has been singled out as the possible source of the breach, as it can be used by healthcare providers to search for Medicare numbers for patients who have lost or forgotten their card.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending July 9:
Surfer who saved the world from WannaCry gets ready for the next big virus
Bloomberg News ~ Gavin Finch ~ 06/07/2017
The 23-year-old who saved the world from a devastating cyberattack in May was asleep in his bed in the English seaside town of Ilfracombe last week after a night of partying when another online extortion campaign spread across the globe.
Physicians say EHRs are a net negative for patients
FierceHealthcare ~ Matt Kuhrt ~ 06/07/2017
The benefits that electronic health record systems provide patients in the form of easy access to information comes at a cost to the doctor-patient relationship, according to a new study.

The slightly delayed Digital Hospitals Handbook and news that Telstra Health had been granted access to the My Health Record system for its HealthNow app may have been the most popular stories on Pulse+IT this week, but out in the wider health and IT communities one story dominated, and that was the Guardian newspaper's discovery that Medicare numbers were for sale in the darker recesses of the internet.
Guardian journalist Paul Farrell was able to buy his own number for the price of a few bitcoins from a cheery-sounding vendor on the dark web, and his resulting story made waves around the country on Tuesday. It doesn't appear that everyone's numbers have been released but Mr Farrell's investigations show that the vendor had made a few tidy sales, numbering about 75 all up.

The Department of Defence will hold a market briefing later this month on the health knowledge management (HKM) element of its JP2060 project, which aims to develop a deployable health capability that can provide acute-level care in combat or disaster zones.
The HKM component, known as JP2060 Phase 4, involves an ICT layer that supports the clinical care component of the capability, including the creation and exchange of health data with garrison health centres through a centralised health record.

110 practices in the IPN group and 70 non-IPN practices have now switched on Precedence Health Care's MediTracker functionality, which allows general practices to supply a read-only summary of medical records to their patients through an app.
Best Practice software users can now also download the installation and registration software through the July data update of Bp Premier. Any practice using MedicalDirector or Zedmed can also offer the service, as can any practice using Precedence's cdmNet platform.
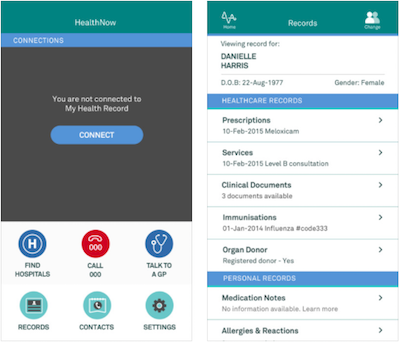
Telstra Health has joined IT systems integrator Chamonix, digital health start-up Tyde and online appointment booking service HealthEngine as a licensed portal operator for the My Health Record, meaning consumers using its new HealthNow app can also access their MyHR through the app.
Chamonix, best known for developing the HIPS middleware solution that is being used by 500 public hospitals and 120 private hospitals to link to the national system and is shortly to go into production to help Sonic Healthcare begin uploading pathology reports, was the the first company to release an authorised app, called Healthi.
The Australian Digital Health Agency (ADHA) intends to streamline the process for healthcare provider organisations wanting to register for the My Health Record, including improving the National Authentication Service for Health (NASH), and is promising to have the system fully automated by May next year.
Announcing a revamp of its developer partner program in Sydney yesterday, ADHA executive general manager for innovation and development Rachel de Sain said the move to an opt-out version of the system had precipitated a fresh look at usability for consumers and clinicians, as well as a commitment to improve the registration and authentication experience of providers.

The possession of a Medicare card number does not give unauthorised people the ability to access the My Health Record, despite some misinformation to the contrary, the Department of Health says.
News Corp newspapers are reporting that yesterday's revelation by the Guardian that Medicare numbers could be bought on the dark net meant hackers had one of the three pieces of information they need to hack the system.

Ascom Integrated Wireless has appointed former sales and marketing director Feargal O’Farrell as its new managing director, taking over from Robert Wood.
Mr O’Farrell has a long history in healthcare ICT and telecommunications, having previously worked for Ericsson and for Integrated Wireless for 10 years before it was acquired by Ascom in December 2013.

The federal government has referred claims that Medicare card details can be bought on the internet to the Australian Federal Police and an investigation launched.
The Guardian this morning reported that it had been able to buy Medicare card details for $30 worth of bitcoins and that the details of at least 75 people had been sold by the same vendor.
GPs can now follow up on referrals they have made for elderly patients to the My Aged Care system, including who is doing the assessment, whether the patient has been referred on for services and if the referral has been closed and why.
Under changes to the system that came into force today, healthcare professionals can also directly refer a patient to an assessor by phone, fax or webform, and they can ring the My Aged Care contact centre with the consent of the patient to find out if they are already receiving aged care services and what kind.

Standards Australia has released the much-anticipated Digital Hospitals Handbook, developed to provide a set of recommendations informing the design and implementation of digital hospitals, both new and refurbished.
While stating that the foundation for a digital hospital is an electronic medical record, the authors argue that it is still early days in the realisation of what might be termed a fully digital hospital. As such, the scope of the handbook has been limited to articulating principles rather than technical specifications.

Integrating the Healthcare Enterprise Australia (IHE) is holding a one-day seminar in advance of the Health Informatics Conference (HIC) in Brisbane in August, focusing on interoperability and connecting healthcare providers to medical devices, diagnostic imaging and clinical photography.
The emerging threats to medical devices such as ransomware and related viruses will be covered in a session led by Flinders University eHealth security expert Trish Williams, who will discuss how to prevent devices from becoming open doors to breaches of hospital systems.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending July 2:
BCS publishes cyber security blueprint for NHS
Digital Health News ~ Jon Hoeksma ~ 29/06/2017
In a new report, the British Computer Society argues that the healthcare sector has struggled to keep pace with cyber-security best practice and with a systemic lack of investment.
Nuance still down after Petya cyberattack, offers customers alternative tools
Healthcare IT News ~ Jessica Davis ~ 29/06/2017
Nuance Communications, a major provider of voice and language tools is still down on Thursday after it was knocked down by the global NotPetya cyberattack on Tuesday.

Coming hot on the heels of our poll from last week that asked whether the very large sums being spent on digitising our hospitals were justified – close to 60 per cent of you said yes – came the news late last week that InterSystems had snaffled the huge contract to roll out its technology for the Northern Territory's public health system.
We always had our money on InterSystems, a relative quiet achiever that has seen real progress with its TrakCare suite, which it markets outside of the US. Trak has had a few other high-profile wins in our part of the world, including for the new hospital at Bendigo and the replacement of a number of best-of-breed systems at Macquarie University Hospital in Sydney a couple of years ago, but this implementation will be watched more keenly than most.

Health Informatics New Zealand (HiNZ) is holding a one-day Cybersecurity in Health conference in Auckland in early August, aiming to provide best practice case studies and immediate advice for health ICT specialists.
The program will cover emerging technologies, recovery and remediation, incident response plans, security and insurance outsourcing, government policies and tactics, security for mobile devices and IoT and practical case studies.

After a decade in which every second electronic medical record implementation seemed to go poorly and clinicians were becoming increasingly resistant to their somewhat dubious charms, the implementation of the Epic EMR at Royal Children's Hospital in Melbourne last year was more closely scrutinised than most.
Taking a big bang approach and in effect moving from paper to digital overnight could have been a disaster, but by all accounts it has gone off with few if any hitches. Now that it has been in place for over a year, some of the promised benefits of going paperless can be measured and they too are looking pretty good.
RCH's chief medical information officer and consultant paediatrician Mike South was a champion of going digital and has been a driving force behind the hospital's equally successful roll-out of a patient portal. But while achieving EMRAM Stage 6 certification for both the hospital's inpatient and outpatient services was a welcome achievement, it is the measurable benefits in terms of quality of care and patient safety that Professor South finds most pleasing.

The Department of Health has complied with the rules relating to the procurement of the National Cancer Screening Register (NCSR) but it could do a little better in keeping conflict of interest records, an Auditor-General's report has found.
The awarding of the contract to Telstra Health – originally worth $178.3 million but later revised up to $220m over five years – has proved controversial, and earlier this year the issue heated up again when it was announced that the project would not go live as planned on March 20 for bowel screening and May 1 for cervical screening.

There has been a slow but steady uptick in consumer and healthcare provider views of the My Health Record as numbers registered continue to grow.
As the system nears five years in operation, with five million consumer and 10,000 healthcare organisation registrations, Australian Digital Health Agency figures show that on average, 10,300 consumers are viewing their record each week.

BreastScreen Queensland (BSQ) expects to go live with a new system that automates the delivery of breast screen results to GPs later this year, replacing the current system in which the results are sent in the post.
BSQ will begin testing the new system in a few months, using existing services offered by a range of secure messaging vendors that are integrated into GP desktop software.
It may have been criticised as clunky and unsafe in the past but the myGov online portal, which provides access for consumers to Medicare, the My Health Record, the National Disability Insurance Scheme and My Aged Care, has received a clean bill of health from the Australian National Audit Office (ANAO).
MyGov was launched in May 2013 and replaced australia.gov.au, which consumers registering for the PCEHR in its first year had to use. Since then, it has added millions of accounts and by November 2016 had 11 million people using it, the most popular service being the Australian Taxation Office.

Brisbane's Metro North Hospital and Health Service has gone live with Orion Health's electronic clinical referrals platform, allowing clinicians and central intake teams to digitally submit, track and manage outpatient referrals across multiple facilities and specialities.
The new platform, which replaces a previous system built in-house, can be extended in future to include community-based referrals from GPs and shared care functionality.
Orion and Metro North announced the contract in April last year. The new system will integrate with Queensland Health's patient administration and scheduling systems through Orion's Rhapsody integration platform, which is being rolled out by Queensland Health to replace its legacy JCAPS-based middleware system.

Western Sydney Local Health District (WSLHD) has extended the deadline for a tender to develop a smartphone app for type 2 diabetes that can integrate with Western Sydney's LinkedEHR GP-controlled shared care planning platform, with a view to an eventual nationwide roll-out.
Part of the Western Sydney Diabetes (WSD) initiative, it is hoped the app will be launched next year and trialled initially with 2000 patients before being commercially scaled up and extended to the approximately 400,000 people in the region with diabetes and pre-diabetes.

User experience strategist Bernard Schokman will lead a masterclass at the dedicated one-day UX conference being held as part of the Health Informatics Conference (HIC) in Brisbane in August.
Organisers the Health Informatics Society of Australia (HISA) recently launched a community of practice for those interested in exploring and learning about health UX and has incorporated the new conference in the annual program for HIC 2017.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending June 25:
Healthcare AI poised for explosive growth, big cost savings
Healthcare IT News ~ Mike Milliard ~ 22/06/2017
Accenture report expects robot-assisted surgery, virtual nursing assistants, workflow tools and more offering huge potential to make patient care more efficient.
Survey: 75 percent of CIOs concerned about incomplete, inaccurate medication data
Healthcare Informatics ~ Heather Landl ~ 22/06/2017
Despite multidisciplinary efforts to improve medication reconciliation, hospital CIOs still report unsatisfactory results, with three out of four concerned that their organization’s medication history data is incomplete or inaccurate, according to a new survey conducted by the College of Healthcare Information Management Executives (CHIME) Foundation.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.