
Auckland-based health technology firm Orion Health has released a new machine learning service to its Amadeus platform, promising to target avoidable readmissions and administrative costs by using more accurate predictive analysis.
Amadeus is Orion's population health management and precision medicine platform, which also has an Analytics module for risk stratification. The plan for Amadeus Intelligence is to combine machine learning with data analysis to help minimise wastage on unnecessary services and excess administration.

Waikato District Health Board (DHB) has gone to tender for an off-the-shelf anaesthesia information system that can integrate with other DHB systems such as iPM and Clinical Workstation.
The new system will move the anaesthesia service off its fully paper-based workflow to digital, from pre-operative assessment and planning through to operating room processes and post-operative care.

Global health IT vendor InterSystems has released a virtual environment that will allow developers to connect to multiple health data sources when testing and developing SMART on FHIR applications.
SMART on FHIR – or Substitutable Medical Apps & Reusable Technology on Fast Healthcare Interoperability Resources – is a set of open specifications that allow developers to integrate apps with electronic medical records.

Melbourne-based medical software and secure messaging vendor Global Health has reported a small loss for the first half of the year as it invests in exploring international markets and the development of consumer and mobile platforms.
While it reported a large drop in revenue from $7.5 million to $3.1m in the same period the previous year, the 2016 figure was boosted by a $5m one-off payment from the South Australian government to settle the long-running licensing dispute over its legacy Chiron patient administration system still used in some country SA hospitals.

ASX-listed pharmacy software vendor Corum has reported a 15 per cent drop in revenue in its half-yearly results, an expected outcome as consolidation within the pharmacy sector continues and major customer Chemist Warehouse transitions from Corum's flagship LOTS Dispense to its own in-house system.
While revenue was down the company's profit was higher than this time last year. Overall revenue was $6.38 million with a net profit after tax of $223,000.

The Australian Digital Health Agency (ADHA) is looking to recruit a new executive general manager for innovation and development to replace Rachel de Sain, who will step down at the end of the month.
Ms de Sain joined the agency in August 2016, shortly after it was established.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending March 4:
Microsoft rolls out cloud-based tools
Healthcare IT News ~ Susan Morse ~ 01/03/2018
While Amazon and Apple are going after the consumer market, Microsoft is focusing on meeting the needs of researchers, physicians, providers, biotech companies and other organizations that use artificial intelligence and the cloud.
Some health employees willing to sell confidential data, survey finds
Healthcare Informatics ~ Rajiv Leventhal ~ 01/03/2018
Nearly one in five health employees (18 percent) said they would be willing to sell confidential data to unauthorized parties, according to a new survey from consulting and services company Accenture.

It's a common tactic of incoming governments facing big budget shortfalls to call for an independent inquiry to investigate the horrors bequeathed by their vanquished foes, and it happens no matter what stripe your political colours.
Tony Abbott federally and Campbell Newman in Queensland were big fans of “commissions of audit”, arranging them as soon as they took government in the high hopes that the blame for all nasty manner of remedial action could be sheeted back to their predecessors.

NSW and Victoria are leading a new national initiative to digitally capture the child health and development data recorded in the different coloured baby books used in each jurisdiction, one of four initiatives that it is hoped will go towards building a longitudinal child digital health record for all Australian kids in the future.
Led by the National Children’s Digital Health Collaborative, the aim is to explore how every child in Australia can have a comprehensive digital health record from the time they are conceived through to their infancy, childhood and into adolescence, and which is readily accessible by parents and healthcare providers.

The three-month period in which people will be able to opt out of the My Health Record is still not yet decided but it will start before September 1, Department of Health officials say.
And contrary to some erroneous media reports, there will be a paid advertising campaign to support the initiative, backed by a communications strategy aimed at healthcare providers.

The implementation of the new Practice Incentive Program Quality Improvement Incentive (PIP QI) has been delayed for another year to allow general practices adequate time to prepare, despite it first being announced in the 2016 federal budget.
The incentive, which requires practices to share de-identified data extracted from their clinical software on certain chronic illnesses as well as vulnerable and high risk groups, was originally designed to simplify the PIP by combining seven existing incentives covering asthma, cervical screening, diabetes, quality prescribing, aged care access, indigenous health and a procedural GP payment into one QI incentive.

ASX-listed health technology firm Jayex is confident it is still a going concern despite a 14 per cent fall in revenue and a flatlining share price.
Releasing its annual report to December 31 yesterday, the company, which earns most of its revenue from its UK arm, admitted that 2017 was a challenging year but its actual losses are less than the preceding period, when it reported a $4m impairment.

Medications adherence software vendor MedAdvisor has reported a 110 per cent rise in revenue over the same time last year as it begins to build on the $9.5 million investment made by healthcare consumables and equipment provider EBOS Group last year.
The ASX-listed Melbourne firm says it now has 2665 enrolled pharmacies and almost one million patients using the platform, and plans to work in the coming year with EBOS subsidiary HPS on a product that may help reduce readmissions to hospital.

GP software vendor MedicalDirector will integrate Healthshare's referrals directory directly into its cloud-based practice management system Helix by the middle of the year, with practices able to use it rather than maintaining their own specialist address book if they choose.
The Healthshare referrals directory has been available on MedicalDirector Clinical's Sidebar as a widget for a number of years, and Healthshare's patient education application was one of the first chosen for the sidebar when it was officially launched in 2013.

Investing in a statewide electronic medical record, closer ties with the Australian Digital Health Agency on the My Health Record roll-out and an immediate expansion of telehealth provision are among the preliminary recommendations from Western Australia's Sustainable Health Review in an interim report today.
The report says WA needs to confront some “inconvenient truths” about its health system, its sustainability and staff morale, including that its track record in the delivery of ICT “has led to large amounts of money spent in areas that has not necessarily supported the system” or improved health outcomes.

Auckland-headquartered Orion Health has launched a full-service cloud-based version of its Rhapsody integration engine, running on Amazon Web Services (AWS) and dubbed Rhapsody as a Service (RaaS).
Orion says RaaS will offer the power of the on premises product with the responsiveness and lower cost of a cloud system, backed up by the computing power of AWS.

Victoria’s largest public health service Monash Health will connect up its hospital ultrasound machines to the SonoReview structured reporting solution from local firm Kailo Medical after a six-month scope of the market.
Monash has signed a five-year agreement with Kailo to implement SonoReview structured reporting for all ultrasound, point of care ultrasound (POCUS) and bone density across the service.

Pathology and medical centre provider Primary Health Care has released more details about the digitisation investments it is making as part of its Project Leapfrog strategic initiative, including its roll-out of MedicalDirector Helix.
Project Leapfrog is the name given to Primary's focus on improving its relationship with GPs, with more flexible contracts for doctors that increases their share of billings, the introduction of appointments and a plan for operational efficiencies through modernisation and digitisation.

Clinical and practice management software vendor MedicalDirector is firmly in favour of recent plans by the RACGP and the Australian Digital Health Agency (ADHA) to put forward a set of minimum standards for medical software, saying it will help moves towards better interoperability.
MedicalDirector CEO Matt Bardsley said an agreed set of requirements or standards would provide assurance to doctors that information sharing was safe. The company recently released a survey of 320 industry professionals, the majority of them practice managers and GPs, gauging their views on interoperability in healthcare.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending February 25:
Leaked Nokia memo says no path forward for ‘struggling’ digital health business
The Verge ~ James Vincent ~ 20/02/2018
Nokia first jumped into the digital health industry in 2016 with its $190 million purchase of French startup Withings.
Paper records, films most common type of healthcare data breach, study finds
Healthcare Informatics ~ Heather Landl ~ 22/02/2018
Interestingly, network servers were the least common location, the study found, but network server breaches affected the most patients overall.

Pulse+IT visited the University of NSW to hear from some of digital health's luminaries on Wednesday, mingling with a gathering of the usual suspects from Australia, as well as numerous international speakers at the inaugural International Digital Health Symposium.
The symposium, organised by the George Institute for Global Health and the Australian Digital Health Agency, followed a two-day talkfest in Canberra on Monday and Tuesday to celebrate the Global Digital Health Partnership, which ADHA hopes will become very important in the digital health scheme of things.

The WA Department of Health needs to ensure a strong governance framework is in place as it transitions to the $408.8 million HealthNext project, which is replacing the much criticised centralised computing services contract with Fujitsu that famously blew its budget by over $80m.
That contract is due to cease on November 30 but according to a report from special inquirer John Langoulant this week, WA Health is yet to commenced transition planning and acknowledges that the timeframes will be challenging.

Waikato District Health Board is now providing hospital clinicians with access to their patients' general practice records with one click in their clinical system, having provided GPs with similar access to hospital records through their practice management system last year.
GP records are being made available through Medtech's ManageMyHealth portal as well as the new Indici PMS implemented in several Pinnacle Midlands practices. Hospital clinicians can access those portals through Waikato DHB's Clinical Workstation.

Telstra has revealed it has sold its 33 per cent interest in IP Health, which markets the Verdi system used by the Peter MacCallum Cancer Centre in Melbourne and Brisbane's Mater Health.
Telstra first took an interest in IP Health back in August 2013 when it was setting up its Telstra Health business, although the investment was made through Telstra Ventures.

Online appointment booking platform MyHealth1st has become the first third-party appointments vendor to integrate with MedicalDirector’s new cloud-based software Helix.
MyHealth1st, formerly known as 1stAvailable, has completed pilot testing and is now available for general practice customers. The company also markets check-in kiosks, a mobile app and automated intelligent recall systems.

Telstra Health has launched a new online marketplace called My Chooser to help participants in the National Disability Insurance Scheme (NDIS) find local providers of healthcare services for their care plans.
The site is currently in a registration phase and is being marketed to providers to list their services. When enough are listed, it will be launched to eligible NDIS participants.

Medication safety expert Neville Board has been named as the Victorian Department of Health and Human Services' new chief digital health officer.
He replaces Paul Cooper, who has been acting in the role since Andrew Saunders stood down in September last year.

Whanganui District Health Board (WDHB) has gone live with the webPAS patient administration system from DXC, replacing the aged OraCare PAS that is now well into its third decade.
Whanganui's roll-out follows similar implementations at MidCentral and Wairarapa DHBs, which went live in December and January respectively. The other DHBs in the Central region will also roll webPAS out in the near future.

North Haven Hospice in Whangarei is providing access to its PalCare electronic record to clinicians and allied health staff from Northland DHB to improve information sharing for palliative care patients.
GPs and practice nurses are already able to view and contribute to patient notes on PalCare, a cloud-based patient management system used by 20 hospices in New Zealand including North Haven, which has been a client since 2004.

The Department of Human Services will end the use of site and individual public key infrastructure (PKI) certificates for healthcare provider authentication by December 2020 in favour of the more secure Provider Digital Access (PRODA) system.
The announcement is part of the federal government's response to the independent review of health providers’ access to Medicare card numbers, which was sparked by the revelation that some numbers could be bought on the dark web.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending February 18:
FDA’s Scott Gottlieb wants to use funding boost to create a Center of Excellence on Digital Health
FierceHeatlhcare ~ Evan Sweeney ~ 15/02/2018
The Food and Drug Administration plans to use a proposed $400 million boost in federal funding to focus on a range of innovative approaches to speed the approval of new medical devices and create a new center that would support digital health oversight and address cybersecurity concerns.
Blockchain not a panacea for managing health records, fed expert says
Health Data Management ~ Greg Slabodkin ~ 15/02/2018
While blockchain has a number of potentially promising healthcare applications, including the management of electronic health records, the technology has certain pitfalls that may inhibit its utility.

Former Northern Territory Health CIO Stephen Moo has taken a role as executive consultant for digital health with Brisbane-based eHealth specialist firm JP Consulting.
Mr Moo resigned as NT Health CIO in September last year under circumstances that are still unclear.
We were vaguely amused this week when, among the voluminous coverage of Victoria's draft regulations for its SafeScript real-time prescription monitoring system, we discovered that federal Health Minister Greg Hunt was threatening to write a sternly worded letter to all the other states and territories to ask them to get a move on with the federal RTPM system that he has championed to the tune of $16 million.
Amused because this is exactly what one of his predecessors, Peter Dutton, did way back in 2014 and no one paid him any attention then either. Four years on from those sternly worded letters, here we are, with Victoria giving up on the feds and building its own system and the ACT government only just announcing last week that it will legislate to give prescribers and pharmacists real-time access to its existing monitoring system by March 2019.

The Department of Health says it is confident the remaining elements for the full roll-out of the National Cancer Screening Register (NCSR) are on track for completion in the next month or two despite hopes it would be ready last month.
The department has also yet to set a date for the start of the new electronic bowel screening program, which was supposed to start in March 2017, telling a joint public accounts and audit committee hearing in Canberra yesterday that the bowel cancer plan will recommence when it has fully delivered the register services, being built by Telstra Health

Data acquisition and analytics specialist Converging Data plans to add an automated response to security events in the next release of its Cyber Security Accelerator (CSA), which is set to be rolled out at a major hospital in Melbourne next month.
Bendigo Health is also using the CSA, which provides security monitoring and response mechanisms for organisations such as hospitals that often don't have a lot of security or IT resources.

Telstra Health has moved to reassure users that it will continue to roll out new releases of its Communicare clinical and practice management system, bringing back founders Brian and Kerry Dunstan to help provide technical support for the software, which is widely used in Aboriginal and Torres Strait Islander communities.
Communicare general manager Anthony Walker, who took over from former GM Greg Robinson in December, has told customers that despite some rumours that there would be no new versions of the software, the company would instead release them on a quarterly basis.

New Zealand's new health minister David Clark has ordered a review into the national bowel screening program following the discovery that some people had not received invitations for screening as their addresses were not up to date.
The roll-out of the new program, which will take a year longer than expected due to difficulties sourcing a suitable IT system, will continue while the inquiry is undertaken, with a report due by June.
A Sydney-based advertising executive has developed an app that helps deliver practical support to people undergoing medical treatment or living with a serious illness such as cancer.
Developed by Rachael Lonergan in collaboration with the Garvan Research Foundation, the CanDo app is designed to help people going through treatment to ask for help with everyday tasks and promises to help coordinate team and task management.

Brisbane's Metro South Health and Hospital Service is weighing up its options for a new patient entertainment solution, going to market for information on choices ranging from a simple replacement TV solution or a full 'patient-centred and interactive health connections solution'.
The scope is initially for the 873-bed Princess Alexandra Hospital but there is the potential to roll it out to the other Metro South sites at Logan, Redland, QEII and Beaudesert.

Alfred Health will roll out mobile workstations at the bedside to provide access to its Cerner electronic medical record as part of its Electronic Timely Quality Care (eTQC) program.
The health service, which includes The Alfred, Caulfield and Sandringham hospitals in Melbourne, has issued a tender for two different configurations of the workstations, one model for doctors and one for nurses that has lockable drawers for medication administration.

Peninsula Health will continue be the sole provider of the Personal Alert Victoria (PAV) service, which provides personal alarm call services to elderly and disabled people living at home, in a deal worth $100 million over nine years.
Peninsula Health has been running the Mount Eliza Personal Alarm Call Service (MePACS), which provides daily monitoring and a 24/7 immediate emergency response service, since 1989. Clients are provided with a Smartlink Medi-Link personal alarm unit and a waterproof pendant.

The Victorian government has released proposed regulations for its $29.5 million SafeScript real-time prescription monitoring (RTPM) system, which will be mandatory for doctors and pharmacists to use after an 18-month introductory period.
Victoria is building its own system rather than use the national electronic reporting and recording of controlled drugs (ERRCD) platform, contracting Fred IT to build, implement and support SafeScript to the tune of $6.67m over four years, with $3.5m going to Fred subsidiary Medication Knowledge to run the prescribing and dispensing data feed.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending February 11:
NHS to offer Skype consultations for new mums affected by mental ill health
Digital Health News ~ Hannah Crouch ~ 08/02/2018
New mums who experience mental ill health are to be given access to consultations through Skype as part of further new investment in perinatal mental healthcare.
Tennessee Hospital’s EHR hacked by cryptocurrency malware
Healthcare Informatics ~ Heather Landl ~ 09/02/2018
Decatur County General Hospital, a 40-bed hospital located in Parsons, Tennessee, has informed its patients about a security incident in which is electronic medical record (EMR) system was hacked, affecting 24,000 patients’ records.

Yes, we know that no one has ever said that and really meant it, but this week has been a tough one to be a clinical software vendor, what with being unfairly maligned by a high-profile medical college, caught up in a state election campaign and otherwise taking the blame for all manner of ills.
Poor old EPAS in Adelaide came in for yet another beating from local rag the Advertiser last week, which reported that 25,000 outpatients were missing an urgency rating following a transfer from the old booking system to EPAS, which clinicians will now have to fix up and are rightly grumbling about.

The funsters behind the popular Smiley customer feedback system have launched a new touchscreen version that will allow hospitals and healthcare organisations to delve deeper into the whys and wherefores of positive and negative feedback from patients.
Used throughout the world and in a number of industries, the technology was developed by two Finnish software developers in 2009 and is used in the healthcare sector to monitor patient satisfaction with elements such as waiting time and communication with clinicians as well as visitor feedback.
The technology is distributed in Australia and New Zealand by Auckland firm Push My Button and is used by Auckland and Waitemata DHBs and Compass Health general practices, as well as Alfred Health in Melbourne and some PHNs taking part in the Health Care Homes trial in NSW.

The Victorian Department of Health and Human Services will roll out NextGate's market-leading MatchMetrix enterprise master patient index (EMPI) technology in a $13 million project also involving Orion Health and MKM Health.
The project is part of Victoria's statewide health ICT strategic framework, which is aimed at modernising IT infrastructure to improve connectivity and also involves Orion and MKM working together on the replacement of existing JCAPS-based integration service with Orion's Rhapsody integration engine.

US laboratory information system vendor Sunquest has officially been named as the winner of the $68.5 million, 10-year contract to replace the 22-year-old Auslab system for Queensland Health.
First revealed by Pulse+IT last year, Sunquest was required to demonstrate a working prototype that would be interoperable with other Queensland Health clinical systems, including its Cerner integrated electronic medical record (ieMR) and its ageing patient administration system.

This week's announcement by the RACGP and the Australian Digital Health Agency of a project to determine minimum functionality requirements for general practice clinical information systems has raised the ire of the medical software industry, with the peak industry association saying no business case had been put forward to support the idea.
The college said on Monday that it would work with doctors and software developers to ensure GP systems are “useable, secure, interoperable, and ultimately fit-for-purpose”, which the Medical Software Industry Association says has been the case for the past 20 years.

It was four years ago that Burwood HealthCare in Melbourne decided to build its own in-house system to allow patients to check themselves in using kiosks that were then new-fangled but are now commonplace, not just in general practice but in hospitals too.
For Burwood, the driving force was a need to increase patient numbers without adding extra reception staff, as the practice couldn't physically fit another person in. Since then, practice owner Peter Demaio and his team have built extra functionality into their system and about two years ago decided to commercialise it, setting up AutoMed Systems and offering the technology to other practices while still using Burwood as the guinea pig.

Brisbane-based precision dosing specialist DoseMe has made its DoseMeRx software available in Epic's App Orchard marketplace, harnessing the power of FHIR and SMART technologies to integrate with the Epic EMR.
DoseMe integrated DoseMeRx as a plug-in app with Cerner's Millennium platform last year and is now working with the third EMR giant, Allscripts, to make it available to its global users as well.

Former Plunket IT manager and Meteorological Service of New Zealand CIO Alistair Vickers has been appointed as CIO of Wellington primary health organisation Compass Health.
In his time with Met Service Mr Vickers led one of the first deployments onto the AWS cloud in the NZ public sector. He also previously did a stint with the Ministry of Health and as CIO of Wellington Water.

The $73 million redevelopment of Latrobe Regional Hospital is now open to patients, with the new cardiac catheterisation lab to open shortly and a $2.6m special care nursery and maternity ward due to be completed early next year.
The project features a new emergency department, doubling the previous capacity, with Allscripts to roll out its Sunrise ED system later this year.

WA's Department of Health is planning to trial the Canadian-developed Artemis platform for early warning of patient deterioration in the neonatal intensive care ward at King Edward Memorial Hospital in Subiaco.
Artemis was developed by Australian-born computer scientist Carolyn McGregor, now based at the University of Ontario Institute of Technology, in partnership with IBM in Canada, where it has been implemented for a number of years at the Hospital for Sick Children in Toronto.

The Royal Australian College of General Practitioners (RACGP) has officially launched a new project aiming to work more closely with medical software vendors to determine minimum clinical software functionality requirements for general practice software.
First announced at the RACGP's eHealth forum in Melbourne last year, the project has the backing of the Australian Digital Health Agency (ADHA) and promises a collaboration to ensure clinical software is "usable, secure, interoperable and fit for purpose".

New Zealand's Southern District Health Board and WellSouth primary health network have launched a new primary and community care strategy that focuses on increasing the use of technology such as telehealth and electronic health records and the implementation of the Health Care Home model of care.
The strategy also calls for an increase in the number of specialist services that are usually provided in either Southland or Dunedin hospitals to being delivered at the community level, starting out as visiting specialist appointments that will over time be routinely accessed in community settings.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending February 4:
Amazon, Berkshire Hathaway and JPMorgan team up to disrupt health care
New York Times ~ Nick Wingfield ~ 30/01/2018
Amazon, Berkshire Hathaway and JPMorgan Chase announced on Tuesday that they would form an independent health care company for their employees in the United States.
Why healthcare interoperability moves at a snail’s pace
Health Data Management ~ Dan Cidon ~ 01/02/2018
Healthcare undoubtedly lags behind other industries when it comes to interoperability. Sadly, organizations remain stymied by systems that fail to communicate. Vendors’ sluggish efforts to make progress have only placed more distrust in the market.

Coming hot on the heels of Apple's announcement last week that it is seriously getting into the healthcare game came another healthcare announcement from a US tech giant this week in the form of Amazon, although what the proposal actually entails is still a bit fuzzy.
The online retailer and cloud provider has got together with Warren Buffet's conglomerate Berkshire Hathaway and financial services firm JPMorgan Chase to explore how to provide healthcare to their tens of thousands of US employees. Speculation initially centred on whether the trio was going to try to take on America's notorious health insurers, but it looks much more likely now that the main game is to explore how technology can cut the cost of healthcare provision.

The Northern Territory will digitise its newly revamped early childhood health record, better known as the Yellow Book, with plans to integrate it eventually with the national child eHealth record app.
The parents of babies born in NT birthing hospitals will be issued with the new Yellow Book from today, featuring extra functionality including space to record vaccinations and consultations and the results for each stage of development.

InterSystems has launched a new unified data platform that it says can make it faster and easier to build real-time, data-rich applications.
The IRIS data platform – IRIS stands for intuitive, reliable, interoperable and scalable – is aimed at any industry that requires real-time analytics on live data from a variety of sources and those looking to consolidate numerous databases.

The Australian arm of standards organisation HL7 International is overseeing a localised version of the interoperability initiative the Argonaut Project, registering Argonaut Australia as a trademark and launching a community consultation on the project's structure and governance.
The Argonaut Project is a private sector collaborative involving major software vendors and healthcare organisations in the US that aims to advance the adoption of standards such as HL7's Fast Health Interoperability Resources (FHIR) and OAuth to improve health information exchange.
HL7 Australia is now launching a local version with the hope of preparing local vendors and healthcare providers for the outcomes of Argonaut, which promise to rapidly improve the interoperability of electronic health records. HL7 New Zealand has been invited to take part and the project has the in-principle support of the Australian Digital Health Agency (ADHA).

NSW Ambulance is testing out the use of ruggedised smartphones by paramedics to tackle mobile blackspots in rural and regional areas.
Under a $314,000 trial, 200 vehicles will be fitted with Sonim XP 8800 devices, which are expected to function more efficiently than satellite phones in many environments and are shock-proof, waterproof and dust-resistant.

About 50 per cent of patients in the greater Wellington region are now cared for by practices taking part in the Health Care Home initiative, with plans to reach 80 per cent of the enrolled Capital & Coast District Health Board (CCDHB) population by the end of the year.
In addition to using Medtech's ManageMyHealth portal to book appointments, request repeat prescriptions and message their practice, patients are now being offered extended assistance such as the ability to talk to their GP on the phone, varied appointment lengths and care planning for those with high needs or at risk.

The NSW government has opened a $6 million cannabis medicines hotline to help fast-track patient access and to help doctors interested in prescribing the medicines.
Based at Hunter New England Health and run with the assistance of the University of Newcastle's Australian Centre for Cannabinoid Clinical and Research Excellence, the hotline will provide advice on clinical management, available medicines and dosage information.

The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) is set to begin a proof-of-concept trial of a mobile antenatal health record nicknamed Digital Babies that aims to digitise the paper records women carry with them through pregnancy.
The pilot will use Global Health's Lifecard personal health digital platform and its integrated ReferralNet secure messaging solution to enable information sharing between specialists and other healthcare providers.

Queensland Health plans to replace its notifiable conditions system (NoCS) for communicable diseases with an electronic disease surveillance system to handle surveillance, outbreak management and contact tracing.
South Australia is also interested in the proposal, with SA Health taking part in Queensland's procurement exercise as an observer to inform its own potential replacement project.

I may be one of the last of a disappearing generation of working GPs. I graduated in 1970, having taught myself to touch type in my sixth year of medical school (which may have been the most useful thing I learned that year.)
I observed the growth of medical computing from that perspective: typed letters, dictated hospital admission notes, the birth of the personal computer, the use of computers to write scripts, then with increasing sophistication to take over clinical recording.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending January 28:
Allscripts offered to buy Practice Fusion for $250M. A DOJ investigation changed everything
FierceHealthcare ~ Evan Sweeney ~ 25/01/2018
Practice Fusion, an EHR vendor once reportedly worth as much as $1.5 billion with goals of going public, sold to Allscripts early this month for just $100 million.
Here's how much top EHR vendors spent lobbying Congress in 2017
Healthcare IT News ~ Bernie Monegain ~ 25/01/2018
Most electronic health record vendors allocated less money to lobbying last year than they did in 2016, with the notable exception being Cerner.

Another day and another tech firm announces they're set to revolutionise healthcare with their dinky new app, promising to bring untold insights from your personal health records to the palm of your hand and enable information sharing on an unimaginable scale. We hear this boast often enough and cast a thoroughly sceptical eye over every one, but when the app comes from Apple, we do admit to taking a little more notice than usual.
Gossip has abounded about Apple's interest in entering the personal health record market for some years and they've already got some runs on the board with their ResearchKit and HealthKit technology and the existing Health app. But while they've been hiring quite a few people with health technology experience over the last few years, speculation about Apple's likelihood of success in PHRs has always been tempered by the example of Google, which tried and failed with Google Health, and Microsoft, which still markets its HealthVault solution but which just this month closed down HealthVault Insights, an app that used machine learning to analyse health data.

Specialist and allied health practices need to be supported in taking part in digital health initiatives such as the My Health Record if the full benefits are to be realised, the Australian Association of Practice Management (AAPM) says, with resources made available to ensure that practice managers across all settings are thoroughly informed about in digital health at the practice level.
In a position paper on digital health released last week, AAPM says there are significant potential benefits that can be achieved through digital health, including better access to care and better health outcomes; improved co-ordination and communication between providers; greater use of data to improve healthcare and influence health behaviours; and economic benefits from system efficiencies.

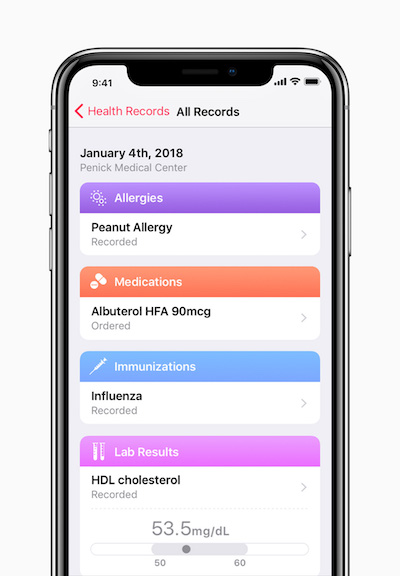
Apple has added a new feature called Health Records to its Health app on the beta version of iOS 11.3 for the iPhone, using the Australian-developed Fast Healthcare Interoperability Resources (FHIR) standard to link hospital medical records to the app.
Apple has worked with EMR vendors Epic, Cerner and AthenaHealth in the first stage of the roll-out, which will enable patients of 12 US-based hospital operators to see their medical data on their phones. All three vendors are part of Project Argonaut, which was set up to develop a FHIR-based API to enable medical record interoperability, and which is coming to Australia this year.

Residential aged care provider IRT Group showed off its Pod Zero driverless vehicle at the announcement of $400,000 in federal funding for the national innovAGEING project today, which will go towards funding plans such as an eight-week innovation program to solve aged care industry problems.
Federal Aged Care Minister Ken Wyatt said the funding would be matched by Leading Age Services Australia (LASA), which is coordinating the collaborative project.

A series of optional two-hour workshops has been added to the program for the 2018 International Conference on Successes and Failures in Telehealth (SFT-18), being held this year in Darwin.
Held in conjunction with the 9th annual meeting of the Australasian Telehealth Society and organised by the ASTS and the University of Queensland’s Centre for Online Health, abstract submissions for formal research and clinical case report presentations are now open, with a closing date of Monday, May 14.

A telestroke service involving Wellington Regional Hospital neurologists providing after-hours advice to less experienced doctors by video conference has seen stroke thrombolysis treatment rates double and firmed up plans to offer it on a nationwide basis.
The service saw a dramatic increase in stroke intervention rates and the service is now being replicated across other parts of New Zealand, with the Ministry of Health developing a new funding model that allows DHBs to subscribe and pay an annual fee based on their individual population catchment area.

Dose Innovations, which distributes the Rowa automated dispensary and inventory management system from Becton Dickinson (BD) to Australian pharmacies, has called in the administrators.
The Brisbane firm, which was set up by pharmacist Robert Allen in 2012 and has installed over 100 robotic systems in community pharmacies around the country, entered voluntary administration last week, appointing Darryl Kirk and Matthew Joiner from Cor Cordis Chartered Accountants to investigate its affairs.

Western Australia's Health Support Services (HSS) agency has issued a tender for an infection prevention and control (IPAC) system to support the surveillance of infectious diseases across multiples healthcare sites in the WA health system.
The proposed solution must consist of a robust data capturing system that will allow for timely management of patients with healthcare-associated infections (HAI); tracking and monitoring of outbreaks and exposures to infectious diseases in the hospital setting; and the provision of valid and reliable data at the local and state levels to monitor trends and the effectiveness of interventions.

Victoria's Austin Health switched on its new laboratory information system last week, the third to go live in a multi-site implementation that also included Peter MacCallum Cancer Centre and Melbourne Health.
The three health services have implemented the Evolution system from Citadel Group, an upgrade to the platform that has long been known as Auslab. Eastern Health has also upgraded its existing Auslab system to Evolution and has renewed its managed service contract to 2023, Citadel Group says.

New Zealand researchers are hopeful that technology developed to identify likely candidates for abdominal aortic aneurysm (AAA) can be further refined and embedded in general practice clinical software to encourage opportunistic screening for the condition.
Developed as part of the Precision Driven Health data analysis collaborative and trialled at the Coast to Coast Health Care clinic near Wellsford on the Northland Peninsula, the project is one of three main areas of interest for Precision Driven Health's Project HOPE (Health Outcome Prediction Engine), the other two being stroke recovery and patient-reported outcomes.

Secure messaging vendor HealthLink has racked up what it says is a significant milestone with 20,000 fitness to drive medical certificates submitted to the NSW Roads and Maritime Services (RMS) agency using its SmartForms technology since the capability went live just over a year ago.
SmartForms allows medical practices to submit clinical documents such as medical certificates and referrals directly from within the user interface of their practice management system rather than going out to an external location or via a toolbar.

Pulse+IT's weekly round-up of international health IT and eHealth news for the week ending January 21:
Study shows little evidence that wearable biosensors aid clinical outcomes
Health Data Management ~ Greg Slabodkin ~ 17/01/2018
While wearable biosensors have the potential to gather health data to support remote patient monitoring, there is a lack of medical evidence that these devices improve clinical outcomes.
ONC: Rise of Alexa, frustrations with legacy systems giving healthcare AI a boost
Healthcare IT News ~ Tom Sullivan ~ 17/01/2018
Artificial intelligence has been hyped as much, if not more, than just about any other major technological advancement in recent history — and that is at least as true in healthcare today as it is elsewhere.

Welcome back to a new year of the weekend edition of Pulse+IT, in which we cast our glance over the events of the week and pontificate for your reading pleasure on what we think it all means for the eHealth and health IT sector. It looks set to be a make or break year for the My Health Record as it goes opt-out at some yet-to-be-decided date towards the end of the year and 20 million people are suddenly presented with a storage receptacle for their health information.
It might be a make or break year for the Health Care Homes project as well, already off to a rocky start with delays and bickering over bundled payments. There was also a bit of a kerfuffle at the end of last year over what shared care planning software the participating practices could choose from and the accuracy of the product information about them.
Team care arrangement have been promoted as the way forward for the primary care sector but actually getting GPs and other members of the care team such as specialists and allied health to use these tools has always been a tough gig. Precedence Healthcare was one of the pioneers of shared care plans in primary care through its cdmNet product, although there are a number of others out there, but even Precedence has found the going tough and shifted its focus once it was acquired by Sonic Clinical Services. It's a struggle for all of these companies, fighting it out for a small market share.

South Australia's Department of Health is looking for a new hospital paging service to replace its 1980s era AEC paging system, covering 10 sites in Adelaide including the new Royal Adelaide Hospital.
SA Health has issued a tender seeking a replacement hospital paging service (HPS) that is based on contemporary technology and which can be effectively integrated with other services and networks such as the Enterprise Patient Administration System (EPAS), the hospitals' Wi-Fi network, and existing PABX and building management systems.

I am 52 years old and a little on the portly side due to an aversion to strenuous exercise and a (in)famous inability to walk past a nice dumpling, pizza, burrito, stir fry or glass of red wine. I have gout, which I am told is genetic, but then again I haven’t met too many skinny, teetotal gout sufferers over my time.
I am starting to feel the first signs of arthritis in my wrist, knees and ankles and I have collected the odd more exotic disease along the way, in my case Gilbert’s Syndrome. I am not sure who the original Gilbert was but it is quite nice to know we at least have something in common.

Clinical and practice management software vendor MedicalDirector and online booking, recall and reminders provider HotDoc have joined forces to offer joint customers the ability to access HotDoc's patient engagement suite directly in their practice workflow.
HotDoc's engagement suite is integrated into Pracsoft and Clinical, and will soon be available in MedicalDirector’s cloud-based clinical and practice management software, Helix.

A new start-up has entered the telehealth arena with the launch of Lysn, a WebRTC-based platform providing video consults to consumers from a bank of qualified psychologists.
Initially founded by Australian doctor Jonathan King in 2016, Lysn now has over 100 clinical and general psychologists on board since its full launch last November and is currently facilitating about 35 consults a week at a fee of $69.50 for 25 minutes or $139 for 50 minutes.
The next big step is to work out a solution to enable patients to claim the Medicare Better Access rebate, which provides GP-referred patients living in small towns in rural and remote areas with Medicare-funded mental health consultations by telehealth.

Problems finding a suitable IT solution to handle New Zealand's $77.8 million National Bowel Screening Program (NBSP) has meant its national roll-out will be delayed by a year, although the six district health boards planning to kick off this year will go ahead using the interim solution developed during the program's pilot, the Ministry of Health has announced.
The ministry issued a registration of interest for the national screening solution (NSS) in May 2017, having chosen telehealth provider Homecare Medical to act as the national coordination centre for the program, with duties including hosting the 0800 number, sending letters to participants and notifying GPs electronically of all results.

The Queensland government has issued tenders for an internal and external eReferrals solution and an online service directory for referring doctors, two key elements of the state's planned statewide integrated Referral Management Solution (iRMS) program.
The intent is to allow GPs to submit referrals electronically to speciality outpatients clinics through their practice management software or from HealthPathways, by 2020, with the first implementation to go live this year, along with an internal patient referrals and tracking system for use within hospital and health services.
iRMS itself is a key element of the $361 million Specialist Outpatient Strategy launched in September 2016 to tackle outpatient waiting lists, which has already seen GPs given online access to their patients' hospital records.

Austin Health and the University of Melbourne are getting together to set up a new Database Analytics Research and Evaluation Centre (DARE) to explore the use of health data to support research.
Austin Health CEO Sue Shilbury said the centre would involve a sophisticated data sharing and storage platform to translate research findings into clinical systems that will improve patient care.

Cairns Hospital has begun transferring paediatric patients' vital signs wirelessly into the state's Cerner integrated electronic medical record (ieMR) using vital signs monitors customised with Queensland's paediatric early warning algorithm.
Called the iVitals system, the hospital is the first in the state to go live with Queensland's Clinical Excellence Division’s Children’s Early Warning Tool (CEWT) built into the Welch Allyn devices.

Former Pacific Radiology Group CEO Lance Lawler plans to address the potential effects of artificial intelligence on the profession during his two-year tenure as president of the Royal Australian and New Zealand College of Radiologists (RANZCR), promising to promote the benefits of AI rather than the hype.
Pacific Radiology is one of 24 organisations worldwide that signed up in 2017 to take part in IBM's Watson Health collaborative to help develop cognitive computing tools in medical imaging.

The University of NSW is looking for NSW-based GPs to take part in a large clinical research study using a personalised smartphone app to help patients with gout to manage their symptoms.
The gout app has been designed in association with GPs and people with gout and tested in a pilot study. This has now moved on to a clinical study of about 560 people.

Sydney-headquartered health informatics firm and EHR vendor Ocean Health Systems will continue to operate on a business as usual basis despite entering voluntary administration last week, with hopes the company can be restructured and work through its financial problems.
Administrator Peter Krejci from insolvency and business recovery firm BRI Ferrier said Ocean would continue to trade during the voluntary administration process, with an examination of the company's affairs to be delivered before a creditors' meeting in about a month's time.

Users of Fred IT's cloud-based solution Fred NXT can now directly access medicines information from the Australian Medicines Handbook (AMH) while they are dispensing through a new app on the Fred NXT app bar.
Fred NXT pharmacies that have a subscription to AMH Online can from today access relevant information about the drugs they are dispensing as they are doing so. Fred NXT has similar capabilities for users of eMIMSCloud and AusDI.

The Pharmacy Guild will shut down the MedsASSIST system it built to monitor over-the-counter combination analgesics containing codeine on January 31, the day before the products are officially upscheduled to prescription only.
The guild initially decided in March last year to discontinue the system after losing the battle to keep codeine-containing medicines on pharmacy shelves, but reversed its decision a day later following the intervention of federal Health Minister Greg Hunt.

It wasn't a good look for online news outlet The Conversation this week when it was forced to retract an article by Deakin University academics Danuta Mendelson and Gabrielle Wolf about the My Health Record. The article was taken down in a flash once several egregious errors were pointed out but is still available online if you search hard enough.
It wasn't a good look for the authors either. It seems they misread the recent legislative rule enabling the opt-out model for the My Health Record to be applied next year and thought it started a fortnight ago. They also seemed to think health practitioners can search for patients' records just with their Medicare number. We suggest that the Australian Digital Health Agency and the Department of Health put their heads together to see how these misunderstandings can be avoided in future.

The roll out of the Health Connect South secondary care system and the primary care portal HealthOne was a notable achievement for the South Island this year, with Nelson Marlborough the last of the five DHBs to turn on HCS in February and local GPs getting access to HealthOne gradually over the next couple of months.
Our interview with NMDHB clinical director of information systems and Nelson GP Bev Nicolls was one of the year's most popular stories. The combined systems now represents a shared electronic health record for one million South Islanders which in future will be opened up to the patients themselves.
New Zealand's primary care PMS market, so long dominated by Medtech, began to fracture and change in 2017, as new entrants like Australia's Best Practice and Irish firm Valentia made some inroads. Canterbury PHO Pegasus decided to go with Intrahealth's Profile to replace Medtech32, with NZ Doctor reporting that it is set to be renamed Sirius, although practices that want to stick with Medtech can do so.

New Zealand readers were most interested in the goings-on with the national electronic health record this year, and we suspect next year as well, when the new government will make a decision on whether to proceed with it or not. With director-general of health Chai Chuah standing down and a new minister in the hot seat, things look likely to get a shake-up in 2018.
In 2017, the national EHR, the adventures of Orion Health and the South Island HCS/HealthOne roll-out were all must reads, as were stories on patient portals and the purchase of HealthLink by the Clanwilliam Group. It was a story on the Ernst & Young report into Health Care Homes that took out top spot this year, although the melodrama that engulfed Waikato DHB was a late contender.

The perennial favourites of Telstra Health and the My Health Record featured strongly in our top 20 most-read stories for 2017, joined by a lot of interest in the various digital health strategies and budget bonanzas for eHealth Queensland and eHealth NSW.
News on movers and shakers was also popular, with two jurisdictional CIOs standing down and one former jurisdictional director-general standing up. DXC and InterSystems also made the list, but the top story was from the primary care sector, where there was huge interest in a little app that promises to do big things.

October got off to a flyer with the announcement that the delayed discussion on the secondary use of My Health Record data was kicking off again. This is one of the most controversial aspects of the national system, and an agreed framework needs to be sorted before the opt-out model can go ahead. An industry survey back in 2015 showed that 64 per cent of respondents believe that individuals need to provide direct consent to the researcher for their data to be used.
Also in October, we had a long chat to the Australian Digital Health Agency's (ADHA) executive general manager for government and industry collaboration and adoption Bettina McMahon about the agency's 2017-18 work program and how it aligned with the national digital health strategy. Ms McMahon explained the thinking around making secure messaging interoperability a priority and explained how the six test beds mentioned in the strategy would fit in. The test beds are two-year programs predominantly driven by the states and territories covering how to encourage emergency departments to use the My Health Record, how digital health can be used to improve residential aged and end-of-life care, and the Collaborative Network for Child Health Informatics, which was announced back in April.

Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.