
South Western Sydney PHN is gearing up to go live in five general practices and three emergency departments with its pioneering iRAD interoperability project, which is using Allscripts' dbMotion solution to deliver relevant patient data in a concise view within clinical workflows to ED clinicians and GPs.
The project is using FHIR-based APIs developed by Victorian firm Oridashi to extract a minimum data set from GP systems Best Practice and MedicalDirector and deliver it through dbMotion to EDs, as well as a dbMotion API to extract data from electronic discharge summaries held in the My Health Record to deliver concise information to the GP desktop.

Victoria is in the market for a vendor neutral clinical information sharing (CIS) solution that can integrate with the different electronic medical records and patient administration systems used by the state's 151 hospitals.
The CIS will also be used to give clinicians access to patients' My Health Record so they can see both local health data and a summary of the patient's medical history held outside the state hospital system.

Labor has called for another Senate inquiry into the move to make the My Health Record an opt-out system, announcing it will ask the crossbench to support a reference to the Senate Finance and Public Administration References Committee.
The move follows intense public debate on the measure, despite a Senate inquiry being held in 2015 and a bill authorising the health minister to move the system to opt-out passing both houses of parliament with bipartisan support that year.

Western NSW has expanded its telehealth in residential aged care facilities (TRAC) program to the small far west town of Wentworth, which joins Broken Hill and Dubbo in offering the service.
The program, funded by Western NSW PHN and the NSW Rural Doctors Network, uses Healthdirect's WebRTC-based Video Call service to improve access to GPs, allied health and specialists for aged care residents.

The Royal Australian and New Zealand College of Radiologists (RANZCR) is holding a summit in Sydney in November to discuss the role of artificial intelligence (AI) and technology in healthcare.
The Intelligence 18: AI in Healthcare Summit will debate the effect of machine learning and big data on healthcare, and will include speakers such as Imperial College London's Yves-Alexandre de Montjoye, an expert in machine learning techniques and analysing and identifying metadata trends.

Primary Health Tasmania (PHT) has issued a request for proposal for a statewide eReferral system that will initially facilitate electronic referrals between GPs and specialists and in future integrate with Tasmanian hospital systems and deliver eReferral letters to the My Health Record.
PHT, Tasmania's primary health network (PHN), is working with the state Department of Health and the Tasmanian Health Service on the project, which is expected to be trialled early next year and will manage the authoring, transmission, receipt and management of eReferrals in Tasmania through an end-to-end electronic workflow.

Pulse+IT's weekly round-up of international health IT news for the week ending August 12: Apple FHIRs up data sharing, 80 US health services link to Apple Health, Google for clinical notes, London goes paperless for scripts, bugs lurk in OpenEMR, Blue Button API, EHR state of play in South Africa, Nova Scotia snoop, Meaningful Use overhaul, CVS MinuteClinic
Apple sees FHIR as way to liberate patient data
Health Data Management ~ Greg Slabodkin ~ 09/08/2018
As healthcare seeks to solve its interoperability challenges, tech giant Apple is positioned to empower data-sharing on a massive scale with consumer mobile apps that use emerging industry standards.
Apple health records project continues to gain provider participants
Healthcare Informatics ~ Rajiv Leventhal ~ 06/08/2018
As of an Aug. 2 update from Apple, approximately 80 provider institutions are on board with the project.

Pulse+IT had hoped to keep our weekend edition a My Health Record-free zone this week considering all of the recent palaver, but it just keeps popping up saying “look at me, look at me” and we find we just can't seem to drag our eyes away.
We hold firm to the belief that the heat over the opt-out debate is dying down somewhat – Google Trends agrees with us, although as you'll see from the poll below, two-thirds of Pulse+IT readers don't – but we did expect an eruption to flare up now and then and it did so this week.

Melbourne's Royal Children's Hospital has configured its Epic electronic medical record to ensure clinical notes are kept short and to the point, has turned off many of its alerts and is not using voice recognition in an attempt to keep documentation to a minimum and hopefully avoid the problem of EMR-linked physician burnout that is plaguing the US health system.
While clinician burnout is a concerning feature of the local health system, it has not yet been tied to the overwork problem facing the US, where the federal government has announced it will introduce a “patients over paperwork” initiative and revise the E/M codes that it uses for medical billing for the first time since 1996.

Electronic medications management capability is now available in 38 hospitals in NSW, with a further 31 due to go live by the end of the year as eHealth NSW picks up the pace of its mammoth eMeds roll-out.
In what will be the largest electronic medical record and medications management implementation in the country, eHealth NSW is now planning to deploy the eMeds module faster, with more complex medications being managed and plans in future to apply the system in the community and outpatients settings.

Specialist health design consultancy Navy Design has launched Design Aid 2018, its annual competition to give an underfunded healthcare project access to free user experience design advice.
Last year's winner was Deakin University, which worked with Navy to conceptualise a non-invasive glucose monitoring app.

The NZ Ministry of Health should give urgent consideration to allowing real-time integration of primary care IT systems with the National Screening Solution (NSS) that is currently being designed to manage the National Bowel Screening Program.
In a report released today, the independent panel reviewing the program found that the ministry needs to continue to monitor the risks posed by the interim solution being used, known as BSP+, and to strengthen project management during the design, build and implementation of the NSS.

Melbourne's Northern Health will roll out NEXA's Q-Flow solution to its specialist outpatient clinics at Northern Hospital, Craigieburn Medical Centre and the Broadmeadows Hospital to help improve patient flow and reduce manual administrative practices.
The solution will include self check-in kiosks and Medicare online patient validation, along with SMS notifications.

ASX-listed Hills has promoted general manager of health sales Andy Hall to the role of health of Hills Health Solutions for Australia and New Zealand.
Hall, who joined Hills in February 2017 as general manager of health sales, previously worked for Rauland Australia in sales and business development roles for its nurse call and patient entertainment businesses.

Brisbane's Metro North Hospital and Health Service (HHS) has completed almost 15,000 telehealth occasions of service having expanded its telehealth portal and introduced the Pexip app to allow for consultations with patients at home, in aged care or with their GP.
Metro North has had a telehealth portal since 2016 as one of a range of initiatives that has seen its long-wait outpatients list by 75 per cent since 2014.

Australia's largest medical imaging provider I-MED Radiology Network has partnered with the Sydney Neuroimaging Analysis Centre (SNAC) to develop novel algorithms that will be deployed on an AI platform to help automate medical image analysis.
I-MED, which processes 4.2 million clinical images annually at its 200 clinics across Australia, will supply the bulk of the project’s de-identified imaging and reporting data to inform algorithm development and validation.
The Department of Veterans' Affairs (DVA) is moving its online services to the myGov platform, allowing veterans the ability to access free mental health treatment, view an electronic copy of their health card and lodge and track claims for compensation.
Current and former Australian Defence Force members can register for the new MyService site and link their account to myGov, which will allow them to use the myGov log-in to access MyService.

Pulse+IT's weekly round-up of international health IT news for the week ending August 5: Patient portal for Northern Ireland, linking ED systems in Virginia, swipe card bill rejected by VA, barriers to data sharing, NHS integrated care record, little value for US GPs in patient portals, Walgreens links patients to providers
Northern Ireland prepares for roll-out of patient portal
Digital Health News ~ Owen Hughes ~ 01/08/2018
A patient portal for people with dementia is to launch in Northern Ireland later this month, as part of the country’s national electronic care record project.
It's not often that we admit that a politician has done a sensible thing but that is what Health Minister Greg Hunt did this week, announcing he would introduce an amendment to the My Health Record act to enshrine a requirement for a court order before allowing law enforcement officials to access the system.
This is already the policy and usual practice anyway and has been for six years, but the 2012 legislation does not makes this explicit. Now, it will. Added to the announcement on Thursday at the COAG Health Council meeting that the opt-out period would be extended by an extra month, and a unanimous agreement that the jurisdictions were committed to opt out, the decision already seems to have already taken the heat off the potential Hindenburg that opt-out was becoming.

The program board overseeing the roll-out of the South Island Patient Information Care System (SI PICS) is aiming at a revised date of August 31 to go live at Christchurch and Ashburton hospitals, having slightly delayed the implementation from its original target.
SI PICS, which is being built by Orion Health and was trialled at Burwood Hospital's outpatients and community clinics, will eventually be rolled out to all five South Island DHBs. It went live in Burwood's inpatient wards in March last year and at Nelson Marlborough DHB in May 2018.

Intrahealth has appointed John Kerry as its general manager for Australia, following the appointment of Peter Mansell to cover the New Zealand market.
Former GM Craig Longstaff is now in a global business development role.


There has been about an eight per cent increase in the use of integrated electronic medical records by Australian hospitals over the last year, led by significant roll-outs in Queensland and two major uplifts at Eastern Health and Peninsula Health in Victoria, according to The Checkley Group MD Bruce Pedersen.
In an update to his 2017 state of the EMR nation, presented at the Health Informatics Conference (HIC 2018) in Sydney this week, Mr Pedersen found that Cerner still massively dominates the Australian EMR landscape with about 90 per cent market share, including the majority of public hospitals in NSW, all of Queensland and a number of large hospitals in Victoria.

eHealth NSW is planning a proof of concept trial using a global trigger tool with its Cerner electronic medical record, and is also looking at incorporating patient-directed discharge letters in the system for a range of diagnoses.
In an update on the NSW eHealth strategy at the Health Informatics Conference in Sydney this week, eHealth NSW CEO Zoran Bolevich said the eMR2 has been rolled out to 159 hospitals so far, with the electronic medications management (EMM) system now live in 39 hospitals.

Launceston-based medical specialist and University of Tasmania clinical associate professor Terry Hannan has won the Jon Hilton award for excellence in primary care informatics at the 2018 Health Informatics Conference (HIC) in Sydney.
Dr Hannan, a visiting fellow at Macquarie University's Centre for Health Informatics, fellow of the International Academy of Health Sciences Informatics and fellow and former president of the Australasian College of Health Informatics, has a long research interest in health informatics and helped to develop an open source EMR used in low and middle income countries including Kenya.

Health Minister Greg Hunt has agreed to amend a section of the My Health Record act to explicitly state that a court order will be required before information can be released to police or government agencies.
Mr Hunt has come under intense pressure to strengthen the legislation, which has been in place for six years and outlines the circumstances under which the system operator can release information to law enforcement officials.
In a statement last night, Mr Hunt said that after meeting with doctors' groups, he would amend the act to reflect current practice.

The states and territories have agreed to harmonise the content of the jurisdictional baby books given to parents to record their baby's growth milestones, part of an initiative to develop a national digital solution that will in future be connected to the My Health Record.
Representatives from the National Children's Digital Health Collaborative told the Health Informatics Conference (HIC 2018) in Sydney yesterday that the agreement was a breakthrough in a long-standing problem in which each state and territory has its own paper book – in NSW it is the blue book, in Queensland the red book, in the NT it is yellow and so on – with different content.

Australia's three peak digital health and health information organisations have come out in support of sharing information through the My Health Record and the government’s decision to make it an opt-out system.
As debate continues on the privacy provisions of the legislation underpinning the system in the three-month opt-out period, the Health Informatics Society of Australia (HISA), the Australasian College of Health Informatics (ACHI) and the Health Information Management Australia Association (HIMAA) have issued a joint statement in support of the MyHR, saying the sharing of patient information is in everyone’s interest and the conversation should be about how to ensure better patient care.

Melbourne-based healthcare software vendor Methsof has entered the hospital market with the launch of HS8, an integrated electronic controlled drug register solution that will be trialled at two Australian hospitals in the near future.
Methsof is best known for software aimed at the community pharmacy sector, including its electronic DD-Book controlled drug register and Meth.D.A for opioid dispensing management.


Global EMR vendor MEDITECH has launched its new web-based electronic medical record platform Expanse on the local market at the Health Informatics Conference in Sydney today, promising to help healthcare organisations to connect patient care across the continuum.
MEDITECH, which counts Ramsay Health Care as its biggest client, went live with its first clinical modules in Australia at Chris O'Brien Lifehouse in Sydney last year.

Pulse+IT's weekly round-up of international health IT news for the week ending July 29: NHS priority on interoperability, AI integrated into EMR, AI for appointments, shared child health record in England, insurer Anthem and Samsung partner on telehealth, GP at Hand resistance, hack aimed at Singapore PM
Interoperability now the top priority for NHS IT leaders
Digital Health News ~ Jon Hoeksma ~ 26/07/2018
An overwhelming 82% of respondents said that interoperability that enabled systems and staff to share information on patients was their highest priority. In the 2017 edition of the survey, the figure was just 51%.
Just as we thought some of the gas was escaping from the My Health Record opt out Hindenburg, yet another drama exploded at the start of the week as the media and the privacy lobby seized on the wording of section 70 of the My Health Record Act, a couple of paragraphs of legalese that is either quite straight forward or a stain on humanity depending on your point of view.
Various interpretations of exactly what s70 means abounded, but it in effect lays out the circumstances under which the My Health Record system operator, namely the Australian Digital Health Agency (ADHA), would be authorised to release health information to law enforcement officials, including the police and the immigration department.

St John New Zealand has added a falls prevention pathway to its new electronic patient record, allowing ambulance staff to refer patients who have had a fall to services that can help avoid further falls in future.
St John began the roll out of its touchscreen electronic patient report form (ePRF) built by Valencia Technologies, in late 2015, and it is now by all ambulance staff across the country.

Victoria's Peninsula Health has gone live with a significant uplift to its Cerner electronic health record, rolling out clinical documentation in inpatient wards and becoming what is thought to be the first health service in Australia to upload a CDA 3A discharge summary to the My Health Record.
The feat is a breakthrough for an Australian hospital and the MyHR system as it means the discharge summary data is coded using the SNOMED CT-AU and Australian Medicines Terminology (AMT) code sets.

The 137-bed St Andrew's private hospital in Toowoomba has signed on to roll out Philips' Tasy electronic medical record (EMR), a web-based system that allows for the management of clinical, organisational and patient administration processes in a single solution.
Tasy is currently used by hospitals in Latin America, the Middle East and Europe, including a number of Brazilian hospitals that have achieved HIMSS' EMR adoption model (EMRAM) stages 6 and 7.

Federal Health Minister Greg Hunt has agreed to strengthen privacy provisions governing the My Health Record system, the RACGP says.
In a letter to members today, RACGP president-elect Harry Nespolon said certain aspects of the My Health Record legislation, including a section on disclosure of information to law enforcement, were concerning.

Health insurer NIB has rolled out a New Zealand version of its Whitecoat healthcare provider search and comparison site, allowing consumers to search through over 10,000 healthcare providers from a range of disciplines, including GPs, specialists, dentists and physiotherapists.
Like its Australian counterpart, which launched in November 2013, the plan is to add online appointment booking and payment capabilities in future.

The Australian Medical Association intends to push again for proper remuneration, including a telehealth MBS item number, for caring for patients in residential aged care facilities.
The AMA is warning of an impending crisis in healthcare for older people as GPs and other medical specialists reduce in-person visits to RACFs due to the amount of time required and lack of suitable remuneration, allied to the decline in registered nurse numbers staffing aged care homes.
The AMA has identified the shortage of RNs employed by RACFs as the biggest priority in aged care reform, with a survey of members saying that having sufficient numbers of experienced nurses available is their top priority. Two-thirds (65.92 per cent) rate this as urgent or extremely urgent.


Australian Medical Association president Tony Bartone will press for a meeting with Health Minister Greg Hunt to discuss how to resolve any ambiguity over the privacy aspects of the My Health Record, promising to do “whatever it takes” including asking for the legislation to be amended if needs be.
The promise comes as opposition leader Bill Shorten calls for the expansion of the opt-out system to be paused, despite the relevant section of the legislation being exactly the same in the original PCEHR Act passed when Labor was in power in 2012 as it appears today.
Dr Bartone told the National Press Club in Canberra today that he had sought and received written assurances from Mr Hunt and Australian Digital Health Agency (ADHA) CEO Tim Kelsey that police and other law enforcement bodies cannot access the system or patient records without a court order or judicial oversight.

Thirty years ago, interoperability was a lot simpler. If you could exchange data between two IT systems, you had interoperability. In the three decades since, the amount of data and the number of sources of data for an individual or a population have both increased exponentially.
Now interoperability is about accessing data across many systems, both inside and outside the organisation, as a single, concordant view, and presenting it to clinicians in a way that is usable and actionable in their workflows.

US-based barcode scanner and printer vendor Zebra Technologies has launched its new range of thermal desktop printers on the local market, featuring new technology that Zebra is calling Print DNA.
The new line of thermal transfer desktop printers and the Print DNA software suite allow healthcare organisations to sense and analyse the status and performance of their printer fleet in real time.

Children's Health Queensland Hospital and Health Service has issued an invitation to vendors to offer a patient online portal (POP) solution, which may in future be rolled out to Metro South and other HHSs.
The POP is a key element of Queensland's specialist outpatients strategy, which calls for patients to be given the ability to manage their specialist appointments online, including access to all of the necessary information relating to that appointment.

Publicly listed pharmacy software vendor Corum will extend live user acceptance testing of its new Corum Clear Dispense solution after hopefully gaining approval for use by the Department of Human Services next month.
A full commercial launch will then follow for the software, which will be accompanied by a suite of products including an updated point of sale module, cloud-based reporting and an expanded set of head office management feature.

Pulse+IT's weekly round-up of international health IT news for the week ending July 22: Blockchain on FHIR with Health Wizz, AI code of conduct, medical device security, ransomware attack on Canadian care homes, NHS telehealth, NHS virtual primary care, EMR global footprint, dodgy mental health apps, EMRs can cut mortality rates
Health Wizz pilots blockchain and FHIR mobile app for EHRs
MobiHealthNews ~ Bill Siwicki ~ 18/07/2018
Health Wizz has updated and is piloting its unusual blockchain- and FHIR-enabled EHR aggregator mobile app, which uses blockchain to tokenize data, enabling patients to securely aggregate, organize, share, donate and/or trade their medical records.
NHS England to publish AI code of conduct
Digital Health News ~ Hannah Crouch ~ 19/07/2018
NHS England plans to publish a code of conduct for the use of artificial intelligence (AI) in healthcare later this year.

One day in the not-too-distant future, communications and business students in universities across the land will sign up for a course called Marketing Disasters 101 and be presented with a case study about the utter train wreck that was the great My Health Record opt-out launch of July 2018.
Pretty much the only thing that could have made this week's debacle worse would have been an actual breach of the system itself. On Monday morning, a huge gang of online activists were just waiting for the clock to tick over to opt out before they let all hell break loose, and my word did they succeed. Social and mass media were dominated in the morning by stories about long delays and system collapses, and by the afternoon it had turned into a veritable production line of tinfoil hats.
One absolute hero got on the phone at 7am to opt out and then for the next few hours martyred himself to the cause by giving 10-minute updates on Twitter about how long he had to wait on the hotline. In the afternoon, he took to claiming that the use of the reCaptcha plug-in on the opt-out website meant everyone's identity verification information was now being flogged off to Google.

A clinical safety review of the My Health Record system has recommended that work be done on a streamlined presentation of the clinical documents contained in each record to help clinicians more efficiently find new and pertinent information.
The review, the tenth such safety review carried out on the PCEHR/My Health Record by the Australian Commission on Safety and Quality in Health Care (ACSQHC) since the system's launch in 2012, found that it is difficult for clinicians to efficiently find clinical information in the My Health Record system using their clinical information systems (CIS).

Public health information service Healthdirect Australia has launched its second voice-activated app, designed to be used with smart devices such as Google Home and Amazon Echo.
The free healthdirect Flu Advice app includes bite-sized information and advice on colds, flu and vaccinations, as well as real-time data about the current flu risk levels in each state and territory.

The four health IT companies that have referred Auckland primary health organisation ProCare to the privacy commissioner have rejected claims by the PHO that the forms patients sign when enrolling in a practice provide adequate consent for their data to be collected.
They have also questioned ProCare's claim that patients have been asked to fill out a new form as a result of the introduction of the National Enrolment Service (NES), a patient register that also provides up-to-date national enrolment and identity data for capitation-based funding (CBF) calculations.

Consulting firm Deloitte has been contracted to undertake a three-month review of NSW Health's Electronic Recording and Reporting of Controlled Drugs (ERRCD) capabilities as part of the move towards a national real-time prescription monitoring (RTPM) system.
The $350,000 contract will see Deloitte report back to eHealth NSW in October with an evaluation of the required business change, ICT delivery approach, and support and governance requirements of the national RTPM and NSW ERRCD capabilities.
An eHealth NSW spokesperson said the analysis will assist NSW Health with future decision making on RTPM.

Melbourne-based GP research network Outcome Health will integrate My Health Record data into the hospital admission risk predictor tool the organisation is rolling out to practices involved in its POLAR project, in one of two digital health test beds it is leading under the Australian Digital Health Agency's $8.5 million test bed program.
It will also work on expanding the POLAR tool – it stands for POpulation Level Analysis and Reporting – to provide a new capability for GPs to visualise what has happened to a patient in a particular amount of time from within their clinical workflow.

The Victorian Cancer Agency has awarded five workforce fellowships worth $300,000 over two years from its cancer health service research program, which includes funds for mobile apps and precision medicine.
This year’s recipients are all women, and they plan to work on projects ranging from the prevention of cancer-associated blood clots to reducing medication errors, developing guidelines for treating cancer-related fatigue and reducing complications from childhood cancer treatment.

A group of four health IT companies, including New Zealand's leading practice management system and secure messaging vendors, have asked the Office of the Privacy Commissioner to look into a new data extraction and storage system run by ProCare that contains identifiable medical data on up to 800,000 Auckland patients.
Representatives from HealthLink, Medtech Global, myPractice and Best Practice NZ have written to the Privacy Commissioner about the data collection, saying they are concerned that patients don’t appear to be aware their medical records are being copied into new databases.

Social media users have complained of long waiting times on the My Health Record hotline and a temporary breakdown in the single sign-on capability of the MyGov site on the first day of the three-month opt out period.
Twitter users who tried to opt out have reported receiving messages that the call centre was experiencing a high volume of calls and others have had problems verifying their identity in order to opt out online.
A spokesperson for the Australian Digital Health Agency said if consumers were not able to get through today, they can opt out over the next three months. The opt-out period ends on October 15, but consumers can still opt out or in at any time.

The Australasian College of Health Informatics (ACHI) has welcomed the move to expand the My Health Record to almost all Australians, saying it had long supported the concept of consumer access to health information.
The college would now like to see the system move to a data-driven model so consumers are able to be involved in the management of their care.
The college said it believed that while there are legitimate concerns about some aspects of the program, near universal coverage and availability will more effectively drive change that the current low uptake.

Pulse+IT's weekly round-up of international health IT news for the week ending July 15: NHS queen of the fax machine, is IHE old hat?, 10 health data breaches examined, insiders not hackers the big breach danger, PDMP in Alaska, health IT vendor consolidation, AI not trusted
NHS world's biggest fax machine buyer
The Telegraph ~ Henry Bodkin ~ 12/07/2018
The NHS is buying more fax machines than any other organisation in the world due to a “stubborn” resistance to new technology, medical leaders have said.
Interoperability experts take aim at ONC Trusted Exchange Framework
Health Data Management ~ Greg Slabodkin ~ 09/07/2018
Tripathi points out that the draft TEFCA includes “old, very cumbersome standards” from the Integrating the Healthcare Enterprise (IHE) interoperability initiative.

There was good news for healthcare's anti-fax advocates this week with the announcement that the Department of Health would finally move to allow GPs to send referrals to the My Aged Care system through their clinical software.
It never made much sense to have phone, fax and webform referrals but not a more suitable route, considering the cost of equipping the My Aged Care contact centre to receive secure messages from any of the four or five vendors on the market wouldn't have been high.
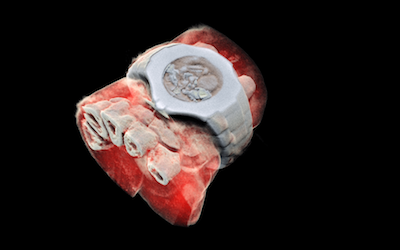
A 3D colour imaging device developed by a Kiwi father and son team is set to go into its first clinical trial for orthopaedic and rheumatology patients in the next few months.
The MARS spectral x-ray scanner is able to produce colour images instead of black and white ones, and show different components of body parts such as fat, water, calcium and disease markers.

Patients living with poorly managed diabetes in north-east Melbourne are being offered new team care arrangements providing them with 24 hour access to their GP medical record through Precedence Health Care's MediTracker app.
Funded by Eastern Melbourne PHN and led by Nexus Primary Health, which runs the GP superclinic at Wallan, and DPV Health, which has two superclinics in Broadmeadows and Mill Park, the new service aims to improve the long-term outcome for people with diabetes and reduce demand on acute services in the area. The superclinics provide allied health as well as medical care.

The Consumers Health Forum (CHF) is surveying consumers about their trust in health apps and whether they think the federal government or some other body should regulate them.
As part of its new Australia’s Health Panel initiative, the CHF has issued a two-part survey asking consumers who they trust to give them advice about a health app, and whether the government should have a system rating apps for accuracy and effectiveness.

A group of researchers and cardiologists from western Sydney plan to investigate the use of My Health Record data to optimise care at Westmead Hospital's rapid access cardiology clinic (RACC) and look at the feasibility of developing a cardiac care app.
The plans form one of 15 digital health test beds that received funding recently from the Australian Digital Health Agency (ADHA), which are looking at using the My Health Record and its data to improve care delivery.
The Western Sydney cardiology care test bed is led by Westmead cardiologist and scientist Clara Chow, known best in mHealth for her work on the TEXT ME trial of SMS messages for reducing risk factors for secondary heart attacks.

Clinical and practice management software vendor MedicalDirector has appointed Petra Gross as its new chief product manager, charged with leading the development of MD's product suite including Helix, Clinical, Pracsoft and Bluechip.
Ms Gross was previously chief product officer at CarsGuide.com.au and has over 18 years' experience in product management, including 15 years in Silicon Valley, where she spent seven years at eBay.

General practices using tools from Pen CS were temporarily unable to log into services in late June following a ransomware attack on the company's externally hosted server, but Pen says the issue was quickly resolved and it is now back to business as usual.
The incident occurred on the morning of June 25 and also knocked out services for the full day of Thursday, June 28. Pen CS assured users that no personal, licensing, practice or patient data was affected and the company does not hold any practice data.

Eastern Melbourne Primary Health Network (EMPHN) is funding free access to after-hours medical care through the My Emergency Dr app for people living in Melbourne’s east and north east in a bid to help reduce unnecessary presentations to EDs.
The app lets patients phone or do a video call with emergency specialists who can order diagnostic tests, write prescriptions, refer patients to other specialists or recommend they attend an ED if needed.

Newcastle not-for-profit ProCare Mental Health Services has won a tender to provide a psychiatry telephone advice service to GPs working in six primary health network catchments in NSW.
The GP Support contract, which has seen the PHNs join together to co-commission the service, can provide advice to GPs managing patients in the primary care setting and is not meant to be a triage or referral service.

The two peak rural doctors' groups have proposed a new model to boost telehealth provision for rural and remote patients, asking both major parties to consider funding a cycle of care arrangement through the MBS.
Developed by the Rural Doctors Association of Australia (RDAA) and the Australian College of Rural and Remote Medicine (ACRRM) last year, the proposal calls for an arrangement in which a patient would see their regular GP fact to face initially, and then be able to receive follow-up consultations by telehealth for both ongoing care for chronic conditions and for routine health checks.

The federal government has finally given in to calls to allow GPs to send electronic referrals to the My Aged Care system from within their clinical software, announcing yesterday it hoped to have the capability available within the next 12 to 18 months.
A spokesperson for the Department of Health said it was currently investigating technology options to enable referrals from clinical information systems directly to My Aged Care, including the use of existing secure messaging services.

WA-based aged and in-home care provider Silver Chain has teamed up with the two Perth primary health networks to develop a new model of care for older people living at home, supported by the enhanced medical mixed reality (EMMR) technology Silver Chain is developing that is delivered through Microsoft's HoloLens device.
The Integrum Aged Care+ trial has received $948,400 from the Perth North and Perth South PHNs' innovation fund and is aimed at reducing hospital admissions and keeping older people at home for longer.

Sydney medical billing, clinical coding and medical transcription specialist Synapse has launched a new rules engine-based app called Synapps MBS, aimed at ensuring Medicare and private health insurance claims are submitted correctly and providing transparency to the hugely complex process of medical billing.
The company, founded and run by well-known medical billing expert Margaret Faux, has also expanded overseas in the last few years, opening offices in Chennai and Dubai to provide clinical coding services to hospitals in the Middle East, many of which have adopted the Australian framework for clinical coding, ICD-10AM.

Pulse+IT's weekly round-up of international health IT news for the week ending July 8: Babylon AI passes RCGP exam, Cleveland Clinic joins Apple Health Records, transmits pacemaker data by Bluetooth, NHS Digital goes De-ID, telepharmacists for meds rec, Humana cyber-spoofed, Vanderbilt adds FHIR to blockchain, Meditech deploys real-time FHIR
Babylon Health says AI abilities ‘on par with human doctors’
Digital Health News ~ Owen Hughes ~ 02/07/2018
Babylon Health claims its artificial intelligence (AI) system has demonstrated diagnostic ability that is “on-par with human doctors” after scoring 81% in a Membership of the Royal College of General Practitioners (MRCGP) exam.

This week got off to a rather officious start when the Australian Digital Health Agency rolled out Health Minister Greg Hunt to belatedly do the honours in officially launching the national digital health strategy and its accompanying framework for action.
The strategy was in fact released last August although it is apparently just now going to kick off, while the draft framework for action was actually released in March and nothing much seems to have changed since then.

ASX-listed health IT firm Alcidion has won a five-year, $4.75 million contract with ACT Health to roll out an electronic patient journey board solution, the first implementation for Alcidion's combined Miya, Smartpage and Patientrack ranges.
The combined solution has been licensed territory-wide and will be rolled out at the Canberra Hospital and the new University of Canberra Hospital as part of the ACT Health Directorate's digital solutions program.
Device Technologies has won a separate contract to roll out the InTouch range of kiosks and flatscreen devices for the program's queue management and electronic wayfinding elements.

The Royal Australian College of General Practitioners (RACGP) has repeated its call for an incentive to be paid to individual GPs for participation in the My Health Record, maintaining its opposition to the practice-based ePIP incentive structure and the upload targets for shared health summaries to qualify.
The college has issued a position statement on the My Health Record this week, as consumer marketing collateral begins arriving to assist general practices with questions they are likely to get from patients about opting out of the scheme. Consumers will be able to opt out online or over the phone from July 16.

ASX-listed Adelaide health informatics firm Alcidion has completed its $12 million purchase of Sydney's MKM Health and the UK-based Patientrack, adding the new assets to its 2017 acquisition of New Zealand clinical messaging firm Oncall Systems.
The combined entity will have established markets in the UK, Australia and New Zealand with its expanded offering. MKM Health provides IT solutions to healthcare providers across Australia and New Zealand and is the local distributor for Patientrack, an early warning system for deteriorating patients that is used by the UK NHS, by four district health boards in NZ and a local health district in NSW.

North Sydney GP Harry Nespolon has won the election to become the next president of the Royal Australian College of General Practitioners (RACGP) and will take up the role at the college's AGM in October.
Dr Nespolon has targeted the Medicare rebate freeze, the return of GP training to the college's control, the controversial planning learning and need (PLAN) CPD activity and remuneration for the My Health Record as priorities for his tenure.
In his campaign manifesto Dr Nespolon criticised the college for signing a deal – or ““compact”, as Health Minister Greg Hunt calls it – with the federal government to end the rebate freeze, calling the move “astonishing”.

A popular branch of technology at the moment is AI, though the name is only half right. It's certainly artificial, but there's not much that's intelligent about it. Automated pattern recognition is a more accurate term because AI systems are getting very good at recognising patterns, but they can't do much else.
Still, pattern recognition is useful. For example, you can drive cars with it. Uber, Tesla and Google are dead keen on building a self-driving future in which our roads will be safer and pleasantly free of congestion. We'll also have more time to look at our devices.

US-based information services firm Wolters Kluwer has launched an advanced version of its UpToDate clinical decision support tool to the local market, featuring interactive algorithms and lab monographs designed to reduce unwarranted variations in care.
UpToDate Advanced features pathways built on current evidence to help clinicians make personalised clinical decisions at the point of care, with an additional Lab Interpretation feature able to help evaluate abnormal test results and decide next steps.
Melbourne-based digital health company IP Health has worked with Mater Health Services to give Mater clinicians access to Queensland Health's The Viewer clinical portal, through its Verdi integration platform.
Mater has used Verdi for many years to provide a clinical workspace with access to data from a number of disparate clinical information systems.

Fifteen projects have been chosen to trial new approaches to healthcare delivery using digital health technologies under the federal government's digital health test bed program, including one involving IPN medical centres and three PHNs that will use Precedence Health Care's MediTracker app to access the My Health Record and GP records for patients with chronic illnesses.
Health Minister Greg Hunt announced the successful bidders at the official launch of the Australian Digital Health Agency's national digital health strategy and framework for action in Sydney today. They will share in $8.5 million in funding to test mature technologies and scale them up for use across the country.

Auckland-based healthcare software vendor Orion Health plans to sells its profitable Rhapsody integration engine business to British private investment firm Hg for $NZ205 million, with some of the proceeds to be reinvested in its population health and hospitals divisions and to fund a share buyback.
Orion will continue to own the hospital division outright, with Hg to take a quarter shareholding in population health, and Orion will retain a quarter share in Rhapsody.

WA-based residential aged care provider SwanCare is rolling out the PainChek facial recognition app, which is able to detect micro-expressions indicative of pain in people with moderate to severe dementia, at one of its Perth facilities with a view to extending its use to home and palliative care.
The app, previously known as the electronic pain assessment tool (ePAT), has now been rolled out to 150 consultants with Dementia Support Australia (DSA), the HammondCare-run centre that provides the federal government's Dementia Behaviour Management Advisory Service and Severe Behaviour Response Teams.

Pulse+IT's weekly round-up of international health IT news for the week ending July 1: Amazon buys into US pharmacy market, Outcome Health's poor outcome, GE spins off healthcare division, transparent Deepmind, US Veterans' EHR, Medtronic and IBM Watson AI for diabetes, Welsh GPs swap preferred PMS, meaningful use v activities-based approach
Amazon's attack on pharmacies has just begun
Washington Post ~ Carolyn Y Johnson ~ 28/06/2018
Online retail giant Amazon is entering the pharmacy business after months of speculation that the company could disrupt how prescription drugs are sold the same way it upended bricks-and-mortar retail.

HealthEngine found itself in a pretty pickle this week when in another bout of bad PR for the online appointments booking service, it was revealed by the ABC to have been flogging off patient contact details to personal injury compensation firm Slater and Gordon.
Exactly what the reasoning was behind developing “referral partnership pilots” with law firms or private health insurers we don't know, but by week's end, HealthEngine CEO Marcus Tan was apologising and promising to review the company's business model for advertising and referrals.

Irish healthcare software vendor Valentia Technologies has launched a voice-controlled virtual assistant that patients using its Indici app can use to book appointments with their GP, request health information or check on when to take their medications.
Indici is a cloud-based practice management system developed in association with the Pinnacle Midlands primary health organisation that has also been chosen as the preferred PMS by Compass Health in Wellington and shortlisted by ProCare in Auckland as part of its PMS review.

The federal Department of Health has issued a tender for the design and build of a national data exchange (NDE) component for the long-delayed national real-time prescription monitoring (RTPM) system.
The federal, state and territory health ministers agreed at the COAG Health Council meeting in April that the national system would run on a federated model, with individual solutions such as Victoria's SafeScript to connect to and interface with the Commonwealth's systems.

WA Health has called for expressions of interest in supplying a customer relationship management app that gives patients a real-time digital record of their outpatient appointment and referral information.
The app will also allow patients to confirm appointments, request an appointment be rescheduled and update their demographic information.

Southern Cross Hospitals and Auckland-based EMR vendor Orion Health have formed a partnership to work together to deliver digital health solutions for the private hospital group.
Southern Cross has almost completed the first phase of its transition from paper to a full electronic medical record, implementing Orion's Clinical Workstation at its 10 wholly owned hospitals and three joint venture hospitals, with one more hospital to come.

Codeine has been added to the list of medications that will be monitored by Victoria's new SafeScript real-time prescription monitoring system, joining a list of prescription opiates, benzodiazepines and sedatives such as Stilnox.
Codeine, which was rescheduled as a prescription-only drug earlier this year, was originally going to be added at a later date but the government has accepted a recommendation that it be included when the system rolls out in October.

Newcastle's John Hunter Children's Hospital has announced it will roll out the Charm oncology information management solution for its paediatric oncology service.
Charm is a best of breed oncology solution used in over 100 sites throughout Australia and New Zealand. It is now part of the Citadel Group following its acquisition of Charm Health last September.

Royal Adelaide Hospital has gone live with a post-anaesthesia care unit (PACU) module following the implementation of a new iPro anaesthesia information management system (AIMS) late last year.
US vendor Allscripts, which has built the enterprise patient administration system (EPAS) for SA Health, partnered with fellow US firm iProcedures for AIMS, which is integrated with Allscripts's Sunrise clinical suite.

The Health Informatics Society of Australia (HISA) has officially launched a new professional development program for executives working in the digital health sector, with planning underway for a certification program.
The Australian Digital Health Executives Network (DHEN) was first suggested by its inaugural chairman Richard Royle (pictured) at the HIC conference in Brisbane last year. It has been formed by a collaboration of senior digital health executives including eHealth Queensland CEO Richard Ashby, Queensland Health's new CCIO Keith McNeil and eHealth NSW CEO Zoran Bolevich.

Deloitte has won a contract to do the initial planning and design for New Zealand's National Screening Solution (NSS), which will initially support the new national bowel screening program and potentially the cervical screening program.
Problems finding a suitable IT solution has plagued the bowel screening program, leading to some people in the trial areas missing their invitation to be screened. The introduction of the HPV test for cervical cancer has also been delayed due to a lack of IT system support.

Online appointment booking service HealthEngine has hit back at claims it provided customers' medical information to private injury law firms surreptitiously, saying it received express consent from users.
It has also rejected claims in an ABC story that consent to share information is hidden in its privacy policies, saying a pop-up consent form is used as part of the booking process and users can still proceed to use the app if they opt out.

The CSIRO's Australian eHealth Research Centre (AeHRC) took out the top award at the Queensland iAwards last week, winning the Queensland Premier's iAward for public sector innovation in addition to the public sector and government category for its mobile-Pulmonary Rehabilitation Platform (m-PR).
It was joined on the winner's list by the Queensland section of the Royal Flying Doctor Service and its partner, app developer Buckham & Duffy, for the HALO aeromedical patient transfer record application, and by Osler Technology for its Clinical Portfolio.

Online appointment booking service HealthEngine has been supplying personal medical information captured from users of its appointments app to third parties, including personal injury lawyers, for targeted advertising purposes, according to the ABC.
The ABC revealed today that it has obtained private documents from law firm Slater and Gordon that show HealthEngine passed on the details of up to 200 people a month during a “referral partnership pilot” last year.

Pulse+IT's weekly round-up of international health IT news for the week ending June 24: Atul Gawande to head Amazon JV, Elizabeth Holmes charged with fraud, NHS GPs up in arms over GP at Hand, Canada rolls out eConsult, Beth Israel to consolidate EHRs with FHIR, Robo-docs and AI, big data in Africa, £20bn boost for NHS
Atul Gawande tapped as CEO of Amazon/Berkshire/JP Morgan Chase joint healthcare venture
Healthcare Informatics ~ Rajiv Leventhal ~ 20/06/2018
Nearly six months after Amazon, Berkshire Hathaway, and JPMorgan Chase & Co announced a joint healthcare venture, the organizations today tapped Atul Gawande, M.D., as CEO of the initiative.

This week in health IT got off to a gallop when we revealed there'd been finally been a breakthrough in secure messaging interoperability after many years of reporting on false starts, but by mid-week, all eyes were on the plummeting returns for Telstra's long-suffering shareholders.
We realised that Pulse+IT is getting a bit long in the tooth when we reflected that we've been reporting on attempts to make secure messaging interoperable since the magazine was established back in 2006. Since then, there have been any number of announcements of breakthroughs: the secure message delivery (SMD) standard, the announcement of the SMX collaboration involving the three main vendors, NEHTA's SMD-POD trials, which promised lots and went nowhere.

HealthShare's directory of private specialists and allied health practitioners will be integrated into the next version of Best Practice's Indigo clinical and practice management software, along with free access to HealthShare’s Referrals directory.
The directory has been available to Bp Premier users as a non-integrated version since 2014. GPs will also have the option to make the directory their default address book for writing referrals inside Bp Premier.

Patients First subsidiary Conporto Health has released an upgrade to its hMael email service for healthcare, allowing customers to send secure emails to non-hMael users.
It has also recently released an event detection and mitigation (EDM) service that its says can provide real-time notifications and alerts to GPs about patients at high risk of medical mismanagement due to poly-pharmacy and co-morbidities.

Gold Coast-based ultrasound specialist Paradise Ultrasound is now uploading diagnostic imaging reports to the My Health Record using its Voyager Imaging suite, the first radiology information system vendor to introduce My Health Record functionality into its medical imaging range of products.
The move means that once a clinical report has been approved by a radiologist, it can be uploaded by the Voyager RIS into the My Health Record system automatically.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.