
Despite the potential of telehealth to provide effective and accessible healthcare for patients, a number of roadblocks and challenges to widespread adoption remain, a recent survey has found.
To the surprise of few in the industry, the five key roadblocks are outdated reimbursement and payment models, cultural attitudes, lack of financial incentives, restrictive policies and inadequate technological infrastructure.
Start-up company Vantari VR will begin trialling its virtual reality technology for patient education and literacy early next year, working with Campbelltown Private Hospital in Sydney to test patient understanding of knee injuries during a consultation with their orthopaedic surgeon.
The Sydney-based company, set up by local doctors Vijay Paul and Nishanth Krishnananthan, is also using the technology at Westmead Hospital for procedural training for junior doctors and medical students, and at Royal Prince Alfred Hospital, where it is being used to render cardiac MRI scans into virtual reality to assist aortic dissection surgery.

Melbourne-based health solutions firm Unified Healthcare Group (UHG) has agreed to integrate its medEbridge platform with life and health insurance claim management software vendor ClaimVantage to allow claims managers to request clinical information from medical practices.
The integration will allow claims managers to search over 50,000 healthcare providers, place orders, track status and receive information back from UHG via medEbridge from within ClaimVantage.

HealthLink co-founder and CEO Tom Bowden is stepping down again, planning to hang out his shingle as an independent consultant to the eHealth sector. His role at HealthLink will be taken by chief financial officer Michelle Creighton.
Mr Bowden co-founded HealthLink in 1993 following a conversation with Orion Health CEO Ian McCrae. The company now has more than 15,000 customers and 100 staff in New Zealand and Australia and is responsible for the exchange of 100 million clinical messages annually.

Lakes District Health Board will join the National Bowel Screening Programme in February next year with Whanganui and Mid Central to join in late 2019 as part of a revised schedule for the national program, the first cancer screening program offered to both men and women.
The NBSP has been delayed in some DHBs due to the time it has taken to develop a new IT system, with the interim system first developed by Waitemata DHB being used by the seven DHBs that are now providing the free program to eligible 60- to 74-year-old people.

The cost for each Queensland Hospital and Health Service to roll out the Cerner integrated electronic medical record (ieMR) has been underestimated and the hoped for benefits of the system have been slow to be realised, but users are generally positive about the system, the Queensland Audit Office (QAO) has found.
The Queensland government estimated in 2016 that the total cost of rolling the ieMR out to 25 hospitals would total $1.2 billion in capital and operational expenditure from its inception in 2011 up to 2025, but the auditor has found that this does not take into account the extra resources the individual HHSs will require.
It also found that the benefits were slower to be realised than expected, and there were differing opinions on whether the decision to use a single vendor rather than explore the market for alternatives is the right one. However, overall the audit found that digitising Queensland's public hospitals is delivering benefits in terms of improving health service delivery and patient outcomes.

US-based medication safety technology firm Tabula Rasa HealthCare (TRHC) has bought Brisbane start-up DoseMe, which makes a precision medication dosing tool that can be integrated with EMRs such as Cerner and Epic.
DoseMe was set up in 2014 by founder and chief technology officer Robert McLeay and its technology is now used in about 100 hospitals and health services around the world. The company set up a US office in June last year and released a US version called DoseMeRx.

The board of HL7 New Zealand has re-elected its office holders following its AGM last week, with chairman Peter Jordan and vice chairman Peter Sergent continuing in their roles.
Eleven of the previous board members were re-elected along with Health Alliance's Karen Blake, who replaces Orion Health's Edwin Ng.

ASX-listed medications adherence technology vendor MedAdvisor has established a 'health services hub' to offer pharmaceutical companies the ability to distribute education and awareness information to target patient groups through its community pharmacy network.
The company has also signed a 50-50 joint venture with Asian pharmaceutical distributor Zuellig Pharma to launch MedAdvisor into the Philippines and South Korea in 2020.

Dementia Australia has got together with Lifeview Residential Care and Swinburne University of Technology to develop an app aimed at encouraging communication between people with dementia and their visitors.
Called A Better Visit, the app includes a number of two-person games that visitors can play with a family member living in residential care who many no longer recognise them or struggle to communicate.

Pulse+IT's weekly round-up of international health IT news for the week ending December 2: Amazon launches NLP tool, Ping An plans unstaffed AI clinics, Apple ECG app to go live, sepsis algorithms save lives, Ghana's mHealth for hypertension, NHS links ambos to mental health plans, $69b CVS-Aetna deal, Canadian genomics platform, telehealth in Alaska, Cerner FHIR APIs live in Oxford, insurer opens EHR to SA patients
Amazon’s latest healthcare foray is a major step into health informatics
MedCity News ~ Kevin Truong ~ 28/11/2018
A new software service from the company called Amazon Comprehend Medical uses machine learning and natural language processing to extract relevant medical information from doctors' notes, clinical trial reports and patient health records
Ping An Good Doctor blazes trail in developing unstaffed, AI-assisted clinics in China
South China Morning Post ~ Yingzhi Yang ~ 19/11/2018
China’s biggest online health care services provider plans to build ‘hundreds of thousands’ of its telephone booth-sized, AI-powered clinics and roll these out across the country in three years.

Those of us with an appetite for the absurd were served up an absolute treat this week by South Australian Health Minister Stephen Wade, who confidently joined the pantheon of comic greats such as Monty Python's hospital administrator who swoons over the machine that goes ping and Yes Minister's manager of the hospital with no patients.
Mr Wade was holding forth in SA's Legislative Council this week on the topic of a turnaround plan devised to extract the Central Adelaide Local Health Network (CALHN) out of a $300 million budget mire it appears to have got itself into.

Auckland's MercyAscot hospital group is aiming to become the first in New Zealand – and perhaps even the world – to fully host its new electronic medical record and patient administration system on Microsoft's Azure Stack hybrid cloud computing platform.
Part of the Healthcare Holdings group, MercyAscot includes two hospitals in Auckland along with Mercy Radiology and Auckland Radiation Oncology clinics.
The company announced in May that it would roll out InterSystems' TrakCare EMR to replace its existing patient administration and clinical information systems, backed by infrastructure support from NZ cloud provider Umbrellar.

Newly reelected Victorian premier Daniel Andrews has announced a new-look cabinet for the next four years, with former minister for families and children Jenny Mikakos taking on the health ministry and the state's ambitious hospital building program.
Former Health Minister Jill Hennessy has been promoted to Attorney General, the first woman to hold this position in a Victorian Labor government. In addition to a number of building projects, Ms Hennessy's tenure as health minister was notable for the introduction of the SafeScript real-time prescription monitoring program.

MIMS CEO Robert Best was elected president of the Medical Software Industry Association (MSIA) at yesterday's annual general meeting, taking over from Extensia's Emma Hossack, who has been in the role for four years.
Joining Mr Best on the board is HealthLink's Tom Bowden, who continues as vice president, and Best Practice's Lorraine Pyefinch, who continues as secretary. The new treasurer is Craig Porte, CEO of aged, community and disability care software specialist carelink+.

Oncology, cardiology and sleep medicine provider GenesisCare will roll out Agfa's enterprise imaging for cardiology platform to all of its cardiology practices in Australia, replacing five legacy picture archiving and communications systems.
GenesisCare, which provides cardiology imaging services in 80 locations across the country, ran a proof-of-concept trial earlier this year and has chosen to proceed with the enterprise imaging system, which in addition to PACS includes structured reporting, advanced image processing and an electronic medical record.

A proof-of-concept trial of the Conporto event detection and mitigation (EDM) solution developed by not-for-profit Patients First has shown overwhelming acceptance from GPs and may even become a requirement for use in general practice in New Zealand.
The system is able to survey a range of clinical systems for potential medication-related harm events and send an alert by email to GPs, triggered by the patient booking an appointment. Details are also sent by RSD message to the GP's practice management system inbox.

Victoria's Barwon Health has awarded a $1.3 million contract to Geelong IT solutions provider Evologic to rebuild its PROMPT document management system, a web-based platform that hosts policies, procedural documents and clinical guidelines.
First developed by University Hospital Geelong intensive care specialist Charlie Corke, PROMPT is now used by over 90 Victorian health services and allows them to search, share and compare policy documents.

The company formerly known as Primary Health Care is in the final stages of negotiation with a supplier for its new laboratory information system, with expectations it will invest around $100 million to deliver the LIS over the next five years.
Now known as Healius following its AGM last week, the company plans to replace the four state-based versions of its legacy Ultra system, first built by Triple G and which is now 25 years old, with a single, integrated system that it says is already in use by a range of pathology operators overseas and in Australia.

ASX-listed Alcidion has won a contract to roll out NextGate's provider registry software to build a statewide referral service directory (RSD) for Queensland Health, which will provide an online directory for GP referrals into Queensland Hospital and Health Services.
A key element of Queensland's statewide integrated Referral Management Solution (iRMS), the roll out will be piloted at Metro South HHS in Brisbane. The solution will also be integrated with the GP Smart Referrals platform being developed by New Zealand firm BPAC Informatics, which will allow GPs to create and submit electronic referrals from their practice software.

Cloud-based medical and allied health practice management software vendor Clinic to Cloud has integrated its platform with Tyro, promising a streamlined payment service for practices and instant Medicare rebates for patients.
Tyro provides credit, debit and EFTPOS services along with Medicare and private health fund claiming and rebating services and offers an integration with Xero's cloud accounting package, which is also offered by Clinic to Cloud.

Primary health organisations Tū Ora Compass Health and the Te Awakairangi Health Network have joined the emerging BeeFound online GP and nurse locum service first launched in New Zealand in June last year.
Developed by Scottish GP Catherine Birchmore and her husband James, the technology behind it has been licensed to Canterbury's Pegasus Health PHO, and is now expanding into the North Island.

Pulse+IT's weekly round-up of international health IT news for the week ending November 25: Finland's health villages, patients to sell own data, Apple's plans for veterans' EHR, Canada Infoway's big idea, US interoperability framework, hacks often inside jobs, DeepMind and Google, Amazon and PillPack, oncology ePROs, Goldacre chairs UK healthtech advisory board
Inside Health Villages, Finland's multimodal digital push to bring healthcare to the home
MobiHealthNews ~ Jonah Comstock ~ 21/11/2018
For the last two years, HUS has been working with a variety of private and public partners to launch Health Villages (Terveyskylä in Finnish), a three-pronged online and mobile platform geared toward bringing as much of the care process as possible out of the hospital and into patients’ homes.
Silicon Valley startup launches blockchain product for patients to sell their data
MedCity News ~ Kevin Truong ~ 21/11/2018
Dubbed PatientSphere, Open Health Network's platform ingests patient data from sources like EHR records, mobile health applications, wearable devices and programs like Apple HealthKit into one dashboard.

Pulse+IT took a trip across the ditch this week to pay a visit to the annual Health Informatics New Zealand conference, where among a terrific line-up of speakers we were lucky enough to hear a ripping yarn from the multi-talented Will Reedy, director of digital for telco Spark NZ, emergency department doctor and independent chair of the advisory committee for New Zealand's national electronic health record (NEHR) project.
Dr Reedy was presenting on the topic of consumer-held records, and it just so happened that on one particularly busy Friday recently at the Middlemore Hospital ED in Auckland, a 60-year-old woman from Boston, Massachusetts, turned up having turned her ankle on a visit to the Cable Bay Vineyards at Waiheke.

Kiwi charitable trust Health Navigator New Zealand is developing a national repository of health-related content that it hopes will enable health organisations to share and repurpose existing content and avoid duplication.
Health Navigator also manages the NZ health app library, which has now reviewed and rated over 100 apps using the mobile application rating scale (MARS) and clinical reviewers.

Australian Digital Health Agency chief clinical information officer Angela Ryan and Wellington-based data governance consultant Karolyn Kerr have been elected president and vice president of the Australasian College of Health Informatics (ACHI).
ACHI is responsible for setting standards for professional practice and education in health informatics and has recently launched a fellowship by training program to support the careers of people entering the digital health and eHealth field.

Auckland-based health technology firm Vensa Health has added two new faces to its 20-strong team along with a global adviser based in the US, as the company reports 20,000 patients using its new vensa.com mHealth platform.
Best known for its TXT2Remind SMS service that general practices use to deliver health message and appointment reminders, Vensa has invested millions into its vensa.com platform, which allows patients to book appointments online in real time and order and pay for repeat prescriptions.

New Zealand's Ministry of Health has finalised a recent restructure that has seen a new directorate for digital and data created, and has also rebadged its national electronic health record project as the National Health Information Platform (nHIP).
Progress on the nHIP, which was first floated at the Health Informatics New Zealand (HiNZ) conference in Christchurch in 2015, has been stalled somewhat since then. An indicative business case was presented to the Cabinet Committee on State Sector Reform & Expenditure Control (SEC) in July 2017, but a request for more detail on its costs and benefits, followed by the change of government last October, slowed its progress.

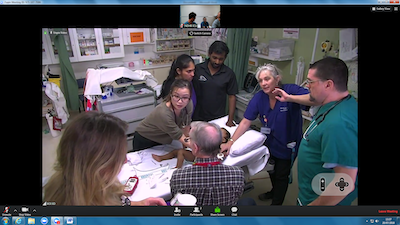
WA Country Health Service (WACHS) is considering extending the emergency telehealth service it provides from its 24/7 Command Centre to also include remote patient monitoring in inpatient, emergency, high dependency and intensive care beds in its network of public hospitals and nursing posts.
The idea is to further develop its existing services by promoting early recognition of patient deterioration at the bedside and in the Command Centre, and to allow patients to be cared for closer to home or on country.
The WACHS emergency telehealth service links emergency doctors in Perth to rural and remote healthcare providers, many of them nurses staffing small clinics where there is no on-call doctor, by video and voice call.

Market leading medical practice software vendor Genie Solutions is investing $6.5 million to develop a cloud-based patient portal for its specialist users, initially featuring pre-treatment forms functionality followed by appointment bookings and billings, and eventually the ability for practices to monitor patient-reported outcomes and experiences.
Genie Solutions, which was acquired by private equity firm IFM Investors in 2017, is also actively on the lookout for opportunities for additional investment to build it into a bigger company, including investing in its core business and potentially in acquisitions.

Clinical and practice management software vendor Zedmed has put its version 30 update into general release after a month-long pilot program, and now plans to shift its development focus to its proposed doctor's app.
v30 of the software features a fully upgraded codebase and a visual overhaul, along with expanded reporting capability, the introduction of surgical procedures lists and support for Victoria's SafeScript real-time prescription monitoring system.

The federal Department of Health (DoH) has dropped a requirement that patients participating in the Health Care Homes trial have a My Health Record, despite it being a centrepiece of the trial model announced in 2016.
The department has told participating practices that it had received feedback that the requirement had caused a small number of potential HCH patients to withdraw their interest, and it may prove a barrier to other patients wanting to participate.

The Townsville, Cairns and Mackay hospitals along with Queensland's North West Hospital and Health Service have got together to trial a telehealth model allowing patients in rural and remote parts of the state to take part in cancer drug clinical trials.
The model, developed by Townsville Hospital and Health Service oncologist and well-known cancer telehealth pioneer Sabe Sabesan, who also runs the Townsville tele-chemotherapy monitoring service, will allow North Queenslanders to have access to drug trials from national and international trial groups.

An already crowded medical school curriculum and no expectation by accreditation bodies that graduates should be able to use digital technologies in practice means the doctors of tomorrow are not being adequately prepared for eHealth, a new study has found.
The study, led by Sisira Edirippulige from the University of Queensland's Centre for Online Health, involved interviews with all 19 medical schools in Australia and is a follow-up to a 2012 study that found that the medical workforce was not being adequately educated to achieve competence to work with eHealth.

Market leading medical software vendor Best Practice Software has organised an online survey to gauge industry and customer opinion about moves by the RACGP to partner with a Canadian vendor to adapt a software solution called Hello Health for Australian general practices.
The move has angered many in the industry, who say it smacks of favouring a newcomer over existing suppliers unfairly, as well as RACGP members, who fear it has damaged the college's reputation.

The Royal Australian College of General Practitioners has rejected claims it undertook an international tour to source new clinical software for the Australian GP market, saying Canadian vendor Myca Health approached it.
The support by the college for Myca Health, a Quebec firm that sells a family practice software package called Hello Health into the US market, has angered many in the local industry, who say they have not been offered the same opportunity to gain the college's endorsement.

The Australian Digital Health Agency has appointed Steven Issa to the new position of chief digital officer, which will see him become the key design authority for national digital health solutions.
Mr Issa is currently director for Service NSW's face to face and digital Service Centres, and is a former deputy mayor and current Liberal Party councillor for the City of Parramatta council in Sydney.

Pulse+IT's weekly round-up of international health IT news for the week ending November 18: What 'Amazon healthcare' could look like, 12 FDA-approved algorithms, messaging apps in emergencies, EMR 'abuse', DeepMind team to join Google, VA EHR using FHIR, $5.7 billion for PMS vendor Athenahealth, FHIR Server for Azure, single log-in for NHS
What 'Amazon healthcare' could look like in 5 years
Health Data Management ~ Yulan Egan and Jacqueline Kimmell ~ 15/11/2018
Over the past year, the company has hired a slew of former healthcare leaders, acquired the direct-to-consumer pharmacy business PillPack, and moved forward with a high-profile venture to jointly manage the health of its employee population alongside JPMorgan Chase and Berkshire Hathaway.
The word 'debacle' certainly got a work-out in the media and on the Senate floor this week as Labor mounted a last-ditch effort to have the opt-out period for the My Health Record extended for a full year. 'Debacle' joined 'bungle' as the words du jour, although we were mightily pleased to see at least one 'shemozzle' and the old favourite 'stuff up' joining the fray.
These choice phrases were of course launched at the government over its handling of the My Health Record opt-out process, particularly as the opt-out website and helpline began to suffer under the weight of people wanting to opt out at the last minute on Wednesday. The government was forced to cave in to pressure to extend the opt-out period, as the amendments to the My Health Record Act demanded by the opposition would not pass the lower house until the opt-out period was over.

Microsoft Healthcare has launched an open source project on GitHub called FHIR Server for Azure, aimed at helping developers to integrate a FHIR server into their application or customise a unique FHIR service.
Microsoft Healthcare general manager Heather Jordan Cartwright said FHIR, first developed by Melbourne-based health informatician Grahame Grieve, was rapidly gaining support in the healthcare community as the next generation standards framework for interoperability.

The South Island Patient Information Care System (SI PICS) being rolled out by Orion Health has gone live at Christchurch Hospital, joining pilot site Burwood Hospital to cover the more than 550,000 people in the Canterbury district.
Nelson-Marlborough Health went live with the new system earlier this year, and the other three district health boards are due to implement the system over the next two years.

The South Australian government has released a tender for the state's long-promised enterprise chemotherapy prescribing system (ECPS), which will be used in the six metropolitan and 15 country SA chemotherapy administering hospitals.
The SA government allocated $5 million in this year's state budget to procure the system, which will be used by about 550 oncologists, haematologists, pharmacists, nurses and clinical administrators.

The federal government has negotiated with One Nation Senator Pauline Hanson to agree to a three-month extension to the opt-out period for the My Health Record, having refused to accept a 12-month delay put forward by Labor.
The Senate this morning heard a number of speeches decrying the government's “botched” roll out of opt-out before Labor moved an extra amendment to the My Health Record Act, calling for it to the opt-out period to be extended to 12 months and for the Privacy Commissioner to review the existing system.

Update: The Senate has rejected an amendment to extend the opt-out period for a year, but has agreed to three months. The opt-out deadline is now January 31.
Labor will move another amendment to the My Health Record Act when it is debated in the Senate today to try to force a 12-month extension to the opt-out period, which is due to end tomorrow.
The move is likely to be successful following a non-binding motion in the Senate on Monday, which saw Labor, the Greens and the cross-bench support an extension by 35 votes to 22. However, the amended legislation will have to go back to the lower house, which isn't sitting until the week beginning November 26.

Private health insurer Medibank has collated patient reported experiences (PREMs) on private hospital stays from more than 30,000 customers and published the data on its website for the first time.
Medibank has been running a patient experience survey since 2016, asking members about nine aspects of their hospital stay, as well as their likelihood to recommend and to rate their overall stay.

The four Northern region district health boards have approached the market for a data sharing and interoperability health information platform (HIP) that will provide the foundations for their regional collaborative community care (RCCC) project, which has replaced the 2016 Northern EHR idea that once envisaged rolling out Epic in both the primary and secondary care settings.
The region's shared services arm healthAlliance has also issued a tender for a regional workspace that will see all systems upgraded to Windows 10 and the roll-out of Office 365, and Auckland DHB has separately gone to market for a patient administration system (PAS) to replace its aged, bespoke system.

The Pharmacy Guild's IT arm GuildLink has rolled out a streamlined method for pharmacies wanting to claim MedsCheck and Diabetes MedsCheck follow-up services through its GuildCare NG professional services platform.
Pharmacies using the technology can now upload eligible patients' medicines profile smart-reports directly to the 6CPA portal. Reminders are created in the calendar after the initial MedsCheck.

The decision by Health Minister Greg Hunt to prohibit health insurers from involvement in the My Health Record system has put the future of Sydney start-up Tyde in doubt, with the company deciding in the next week whether to continue or to wind up.
Tyde has developed a mobile platform that allows consumers to access their My Health Record through an app and to link health records from disparate sources together. It has been in trials with a number of care co-ordination groups including insurers to use the platform to support consumers with chronic health conditions.

Pulse+IT's weekly round-up of international health IT news for the week ending November 11: AI could help meds decision making, AI might not help data analytics, doubts over Babylon's AI claims, FDA rules not sufficient for medical device security, IT overconfident about medical device security, medical transcription vendor booted, pathology joins Apple Health records, EMIS buys into blockchain, mHealth platform for HIV, NHS to gut digital teams
AI system predicts billions of potential side effects from drug combinations
Health Data Management ~ Greg Slabodkin ~ 08/11/2018
An artificial intelligence system developed by researchers at Stanford University could ultimately help physicians make more informed decisions about which medications to safely prescribe.
AI falls short when analyzing data across multiple health systems
Healthcare Informatics ~ Heather Landl ~ 07/11/2018
Artificial intelligence (AI) tools and machine learning technologies hold the promise of transforming healthcare and there is ongoing discuss about how much of an impact AI and machine learning will have on the practice of medicine and on the business of healthcare overall.

This week in the eternal drama that is the My Health Record we were served up a veritable smorgasbord of beat-ups, cave-ins and knee-jerk reactions about the system that would have tested Mr Creosote's enviable staying powers.
There was a story about the whole system crashing under the weight of people rushing to opt out – we have it on good authority that it did no such thing – that was then picked up by other outlets and beaten up within an inch of its life.

It may have flown under the radar somewhat but when the $2 billion, 488-bed Northern Beaches Hospital opened its doors last week, the Healthscope-operated public and private hospital in Sydney's Frenchs Forest went live with a fully functional electronic medical record from Telstra Health.
The Northern Beaches EMR is put forward by Telstra Health managing director Mary Foley as an example of how the company is about to emerge from its blue sky phases of mergers and acquisition and internal restructure into the integrated health information platform provider it always proposed to be.

New Zealand aged care provider BeGroup is rolling out the hands-free Vocera communications badge at its new retirement village in Auckland and will integrate it with a tablet-based communication tool to allow residents to call for assistance through the device.
Rāwhiti Estate caters for independent living and residents requiring rest home, dementia-specific and hospital-level care.

The federal government will accept most of the amendments put forward by Labor to strengthen the My Health Record Act, including increasing penalties for improper use and tightening up the ability for estranged parents to access their child's record to safeguard against domestic violence.
The government has also agreed to conduct a review into the situation for mature minors and parental access to a teenager's record, something the Royal Australian College of General Practitioners has been requesting for over six years.

Children's Health Queensland Hospital and Health Service (HHS) has awarded a $40,000 contract to IT recruitment specialist Harvey Nash to help it source, assess and hire a chief digital officer.
The statewide health service includes the newly renamed Queensland Children's Hospital in Brisbane and community and mental health services, as well as working with the other HHSs on paediatric care.


ASX-listed Adelaide firm Alcidion has won a contract with ACT Health to roll out its Patientrack Bed Board module at the new University of Canberra Public Hospital (UCPH).
It will form part of ACT Health's electronic patient journey board project, for which Alcidion is supplying its Miya Flow, Smartpage and Patientrack technologies.

The Tasmanian Health Service (THS) is updating its open disclosure framework to add breaches of confidentiality through its digital medical record (DMR) to the policy.
Open disclosure usually concerns clinical adverse events that cause harm to a patient, and is covered by a national framework developed by Australian Commission on Safety and Quality in Health Care that provides guidance on how to communicate these incidents with patients.

BreastScreen NSW has begun a phased introduction of electronic delivery of BreastScreen results to GP practice management software using secure messaging.
BreastScreen NSW hopes that in future the vast majority of results, except for patients who have undergone a biopsy or who require surgical management, will be delivered directly into the GP's PMS if the woman has provided her GP's details.
The four Northern region district health boards are progressing rolling out a cloud-based telehealth service using the Zoom enterprise video communications solution, which is being used for virtual patient care, remote specialist visits, and education and care co-ordination.
Assisted by the Northern DHBs’ shared IT service provider healthAlliance, the telehealth service involves a unified video, audio, content sharing and chat platform.

Pulse+IT's weekly round-up of international health IT news for the week ending November 4: 420,000 join Apple heart study, healthcare's most wired, US Medicare to cover telehealth, mandatory breach notification in Canada, HIEs connect to Military Health System, Cerner opioid toolkit, Cerner progress with DoD, AI for sepsis, certified EHR tech
Apple Watch heart study with Stanford signs up 400,000 people
Bloomberg ~ Robert Langreth ~ 01/11/2018
More than 400,000 people have signed up for a Stanford University study being sponsored by Apple Inc. to examine whether Apple Watch can detect patients with undiagnosed heart rhythm problems, one of the largest heart screening studies ever to be conducted.

It's a big bad bungle after a database debacle after a computer catastrophe! No, not the My Health Record – this week it's the Cerner integrated electronic medical record (ieMR) that is rolling out in Queensland that is the topic of some over-excited headlines.
While Pulse+IT had a relatively sedate story this week on the Sunshine Coast Hospital and Health Service postponing its roll-out of the digital hospital stack until next year because clinicians aren't quite ready for it yet – a sensible move, if you ask us – over at Channel 9, things were getting a little heated.

The Western Sydney Local Health District plans to trial the use of wearable devices monitored by clinicians to improve the care of young people with severe mental illnesses.
The unWired project will see FitBit-like personal wearable devices used by young people to measure their activity and level of stress, with data sent back to the wearer and their treating clinician through a purpose-built app.

The new owners of the Rhapsody integration engine built by Orion Health have completed the separation of the company from its parent, taking up new headquarters in Boston with a former McKesson partner as CEO and plans to increase its workforce by 40 per cent in the next 18 months.
Orion Health, which still has a 24.9 per cent stake in Rhapsody and will remain as an investor and reseller of the product, now plans to turn its attention to stabilising and growing its population health management and hospitals businesses while laying the foundations for precision medicine, which chairman Andrew Farrier said the company believed will transform the healthcare sector.

The Australian health information workforce is predominantly female, highly educated and getting older, but few are taking up extra credentials and half do not belong to any form of industry or professional organisation.
Nearly half of all health information professionals are planning to leave the workforce entirely within the next 14 years, which has ramifications for future workforce planning in the overall health sector, which is itself become more reliant on digital health data to deliver patient care.

The Australian Digital Health Agency plans to begin its public consultation on the road towards health sector interoperability in February 4 next year, with a draft set of standards scheduled for release at the end of the financial year.
The agency also plans to ramp up its work in getting the aged care sector connected to and using the My Health Record once the opt-out period finishes on November 15, with plans to work on device integration with the system as well as providing real-time access to clinical registries such as the rheumatic heart disease register for Indigenous health.

Pharmacy software vendor Corum has received its notice of connection to the My Health Record from the Department of Human Services (DHS) for its LOTS Dispense system, used by around 1000 pharmacies in Australia.
Corum will now begin contacting LOTS pharmacies that have registered with the My Health Record to get them up and running with the system.

The planned roll-out of Queensland Health's integrated Electronic Medical Record (ieMR) system at Sunshine Coast University Hospital (SCUH) and Nambour Hospital has been delayed until next year after talks with clinicians.
The digital hospital version of the ieMR at SCUH, which Queensland Health says is the most complex roll-out in the state, was due to go ahead this month, with Nambour to follow in November.

eHealth Queensland is planning to run a proof of concept trial of a digital medical translation solution to supplement its human interpreters when they are unavailable.
eHealth Queensland says that while there are a number of software translators available, none of them have been endorsed for use within Queensland Health, so the idea is to develop and test an accurate medical translation solution in both written and verbal forms. Existing products can be used or modified to provide an appropriate solution.

Hamilton-based shared services agency HealthShare has gone to market on behalf of the five Midland District Health Boards for a clinical portal imaging interoperability solution that will provide clinicians across the region with a view of patient imaging studies from the existing picture archiving and echocardiography reporting solutions.
Part of the overall Midland Clinical Portal program, the preferred solution is expected to also integrate with private radiology and cardiology in the future, along with other imaging modalities such as coronary angiograms, cardiac CT, cardiac MRI and nuclear medicine.

Assistive technology and home monitoring provider Tunstall has released a new version of its Integrated Care Platform (ICP) platform, including a new interface for the myMobile app and the ability for patients and clinicians to send secure messages from within the platform.
ICP is used for a number of home monitoring programs in Australia and the UK, with one community care program currently being delivered in New Zealand.

Victoria's Bass Coast Health has rolled out the MasterCare electronic medical record from Global Health to its specialist and allied health outpatients departments, community nursing and alcohol and drug recovery services.
MasterCare is being used as an EMR and for billing, scheduling and rostering, as well as its data collection and reporting capabilities for a host of government programs and minimum data sets, including the Commonwealth Home Support Program (CHSP), Home and Community Care (HACC), Community Health (CH), Victorian Alcohol and Drug Collection (VADC) and Victorian Integrated Non-admitted Health (VINAH) data sets.

The Pharmacy Guild's IT arm GuildLink has partnered with medications adherence app developer Perx Health to offer a free program to patients taking the Parkinson’s disease medication Stalevo.
The idea is to support patients to form healthier medication habits and improve medication adherence through a digital behaviour change program available at GuildCare NG pharmacies.

Pulse+IT's weekly round-up of international health IT news for the week ending October 28: Trump signs opioid bill, HIMSS infrastructure adoption model, NHS digital test beds, blockchain use cases, patient-reported outcomes, integrating Choosing Wisely into EMRs, making FHIR a requirement
Trump approves opioid package, expands telemedicine, regulates e-prescribing for opioids
MobiHealthNews ~ Laura Lovett ~ 25/10/2018
In one of the few and far between bipartisan bills to be passed during this administration, President Donald Trump signed into law yesterday a new package aimed to help tackle the opioid epidemic, called the Support for Patients and Communities Act.

The My Health Record was back in the news this week as Department of Health and Australian Digital Health Agency officials were forced to undergo yet another gruelling bout of interrogation from the same Senate committee that put them through the wringer not six weeks ago.
Having handed down a report last Thursday recommending that the My Health Record opt-out period be suspended or extended for another year – an idea that was promptly rejected by Health Minister Greg Hunt last week – the same faces fronted up to Senate Estimates on Wednesday, with the same result. The only news was that about 240,000 more people had opted out since the last time the question was asked.

Melbourne's Royal Children's Hospital is using the big data sets it is generating from its Epic electronic medical record to look at areas highlighted by the Choosing Wisely initiative as being care of low value, including the unnecessary ordering of chest x-rays and medications such as antibiotics and anti-asthmatics in babies with the viral infection bronchiolitis.
RCH, which went from a mainly paper-based system to a fully electronic medical record when it implemented Epic in 2016, has received a grant from Better Care Victoria to study five areas of low-value care highlighted by the Royal Australasian College of Physicians' paediatrics and child health division, and is now at the stage of being able to develop targeted interventions to reduce unnecessary tests and prescribing.

BPAC Informatics has won an $8.3 million contract to integrate its SeNT eReferrals solution with Queensland Health's statewide integrated referral management system, allowing GPs to send referrals from their practice management systems or HealthPathways directly to public hospital outpatient settings electronically.
The solution is one component of the statewide eReferrals project, which is itself a key element of the $361 million Specialist Outpatient Strategy launched in September 2016 to tackle outpatient waiting lists, which has already seen GPs given online access to their patients' hospital records.

Primary Health Care will roll out MedicalDirector3, now known as MedicalDirector Clinical, to any of its clinics not currently using it as part of its Leapfrog program, with the implementation of MedicalDirector's cloud-based system Helix still in its future plans.
Speculation has been rife in the industry that Primary had changed its mind on installing Helix in all of its practices, as announced in its digital strategy in 2017.

The federal government will not accept a recommendation made in last week's Senate committee report into the My Health Record that the opt-out period be extended, arguing it was important that people experienced the benefits of the system as quickly as possible and they could opt out in future if they wished.
So far, 1,141,700 people have opted out of having a record, which represents an extra 240,000 opt-outs in the last month. The first two months saw 900,000 people opt out.
Department of Health deputy secretary for health systems policy Caroline Edwards told a Senate Estimates committee hearing that the slowing trend was expected.

Sydney Children's Hospital Network is running a proof of concept study analysing real-time data from its electronic medical record on paediatric oncology patients and their risk of infection.
The aim is to see if it can assist clinicians in their decision-making on whether patients presenting with febrile neutropenia need to stay in hospital for a dose of antibiotics or if they can be better cared for at home. The hope is to also apply the process to bronchiolitis and sepsis in future.

Melbourne-based pharmacy software specialist Fred IT was won a contract with the federal Department of Health to design, build and implement a national data exchange (NDE) service to underpin the eventual roll-out of a federated system of real-time monitoring of prescription drugs.
Fred, which is half-owned by the Pharmacy Guild and half by Telstra Health, is also behind the design and build of the SafeScript real-time prescription monitoring system currently being piloted in western Victoria. It markets the eRx prescription exchange service and the Fred Dispense and Fred NXT suites of pharmacy dispensing software.

Former Orion Health general manager Kate Reid has joined Deloitte NZ's consulting service as a director of digital health, based in Auckland.
Ms Reid, who spent three years with Orion and is the chair of New Zealand Health IT (NZHIT), will be working with Deloitte’s health sector leader Thorsten Engel to expand the firm's offerings and services to the industry.


WA Primary Health Alliance (WAPHA) has supported the roll-out of HappyOrNot smiley face terminals from Auckland firm Push My Button at 45 general practices throughout the state as part of its comprehensive primary care program.
WAPHA operates the three West Australian primary health networks – Perth North, Perth South and Country WA – and is using the terminals to help practices with their quality improvement.

ASX-listed medical centre, pathology and diagnostic imaging provider Primary Health Care plans to change its name to Healius to reflect the change in focus it has had since the end of the Bateman era.
The company will take the name change to its shareholders for their approval at the company's annual general meeting in Sydney on November 22.

Independent accreditation provider Quality Practice Accreditation (QPA) has launched an online self-assessment tool aimed at helping general practices and other healthcare providers understand the requirements of the RACGP standards for accreditation.
Connect Plus can also be used by practice management consultants or accreditation managers from primary health networks (PHNs) as well as by specialist practices.

Pulse+IT's weekly round-up of international health IT news for the week ending October 21: NHS needs £13b for IT, digital health playbook, UK minister outlines NHS IT vision, FDA and DHS on medical device security, Ada speaks Swahili, app for TB, Canadian snoop, $1b telehealth fraud, Anthem pays up, WannaCry cost NHS £92m
Officials' £13bn funding ask to modernise NHS IT
Health Services Journal ~ Ben Heather ~ 15/10/2018
The sum would be on par with the National Programme for IT, the most expensive push to improve IT systems in NHS history and an infamously costly and troubled project.
AMA launches digital health implementation playbook
MobiHealthNews ~ Laura Lovett ~ 17/10/2018
The new playbook will include a step-by-step approach to implementing digital health tools, as well as best practices and other resources.

This week Pulse+IT travelled to Canberra for the Australian Association of Practice Management (AAPM) national conference.
With practice managers typically quite influential in the information technology purchasing decisions made by practices, IT has always featured strongly at AAPM conferences, and this year was no exception.

University of Auckland public health researcher Simon Thornley has launched a study to investigate the use of New Plymouth firm Firstcheck's smartphone app and dermatoscope to help detect scabies.
Dr Thornley's research has shown that not only can misdiagnosis of scabies often lead to complications such as bacterial skin infections, infestations of the mite are also common in areas with high rates of rheumatic fever and rheumatic heart disease.

The Senate community affairs committee looking into the My Health Record system has recommended the opt-out period be extended for a further 12 months, along with a host of further regulations to increase privacy.
The Coalition Senators on the committee issued a minority dissenting report, saying they did not support the year-long extension and calling it “excessive and unnecessary”. They noted that the decision on opt-out was supported unanimously in 2015.

The federal Department of Health should consider whether the $220 million National Cancer Screening Register contract should be terminated or penalties sought from vendor Telstra Health following the costs incurred from a delay in rolling out the system.
A Senate budget estimates inquiry into the contentious contract heard earlier this year that Telstra Health had only been paid $11m of the full $220m cost due to a number of missed milestones for the cervical cancer screening register, which has also delayed the roll-out of the bowel cancer screening register.

Queensland Health has made the unusual move of issuing a restricted tender for the replacement of its 30-year-old HBCIS patient administration system (PAS), inviting just five multinationals to bid for the massive project, which is expected to cost more than $200 million and is hoped to be in place by 2023.
Pulse+IT understands that the five invited firms were Cerner, which also has the contract for the state's electronic medical record, DXC Technology, which maintains the existing system and also markets the widely used iPM and webPAS products, along with EMR vendors InterSystems, Allscripts and MEDITECH.

The Victorian branch of the AMA has called for a commitment by the state's hospitals to work towards the ability to receive and send secure electronic communication to and from the medical software platforms of referring doctors as part of its wish-list for the coming state election.
AMA Victoria also wants to see the introduction of a statewide centralised waiting list system for specialist outpatient services, calling for greater transparency on waiting times.

The federal government has agreed to fund a national trial of a touchscreen-based mental health screening tool for Aboriginal and Torres Strait Islander mothers-to-be as an alternative to the Edinburgh postnatal depression scale (EPDS).
The Murdoch University-developed Baby Coming – You Ready? project has moved from a paper-based assessment to a digitised one that contains culturally appropriate touchscreen images.
The Murdoch team showed in the early stages of the research that indicators used to identify peri- and post-natal depression were not culturally appropriate for many Aboriginal women and failed to identify those at risk.

Allscripts has enabled a read-only view of the My Health Record for clinical staff in 26 metro and country WA hospitals through its BOSSnet electronic medical record.
While many other jurisdictions are using middleware such as the HIPS system developed by Adelaide firm Chamonix to connect to the national system, the Core Medical Solutions team at Allscripts has developed components that enable BOSSnet to directly integrate with the My Health Record and the Healthcare Identifiers (HI) Service.

Auckland-headquartered clinical information system vendor Orion Health has launched a secure health data store built on Amazon Web Services that can provide healthcare organisations with a platform for data analytics, machine learning, value-based care and population health management.
Using its Amadeus big data platform, Amadeus CORE is aimed at helping organisations to store and analyse large quantities of health data from multiple sources. It also enables a system of apps using web APIs that can be used to build applications on top of shared data.

Australia's Department of Defence will replace its EMIS-based primary care clinical information system in the first stage of the massive JP2060 Health Knowledge Management project, which will eventually see the defence force build a system for deployed and garrison staff that reaches at least level five on the HIMSS EMR adoption model, at an expected price tag of between $150 and $350 million.
Defence plans to use a systems integrator from a panel of 28 multinationals to subcontract medical software vendors for the project's requirements, beginning with an off-the-shelf primary care medical record and practice management system and eventually building a full HKM solution for both the garrison and deployed environments.
The first phase of project will see the existing Defence eHealth System (DeHS), which uses the UK's EMIS practice management system and was rolled out by DXC Technology in 2014 with a $56 million budget, replaced. Defence says that system is already reaching the end of its technical life.

The Senate community affairs legislation committee looking into a bill aimed at strengthening the privacy provisions of the My Health Records Act has recommended it be passed, although Labor says it plans to move extra amendments.
While Labor and the Greens supported the recommendation, both parties said the changes were inadequate. Labor also repeated its call for the opt-out process to be suspended until all remaining concerns are addressed.

Pulse+IT's weekly round-up of international health IT news for the week ending October 14: £4.2b for planless paperless NHS, epic Epic install at Mayo, US DoD Genesis roll-out, governing FHIR, tools for nursing shortage, preventing cybersecurity doomsday, health IT policy for opioid crisis
MP's 'horror' at getting £4.2bn to digitise NHS with no plan
BBC ~ Brian Wheeler ~ 02/10/2018
A former minister has described his "horror" at being handed £4.2bn to create a "paperless" NHS in England by 2020 without a plan how to do it.
Mayo Clinic completes Epic install at remaining campuses
Health Data Management ~ Greg Slabodkin ~ 10/10/2018
Overall, the Mayo Clinic took about three years to complete the health IT modernization project at a price tag of approximately $1.5 billion.

Last week, we asked readers whether they thought a local axe the fax campaign, based on a similar one launched in the UK to rid the NHS of its fax machines, would work on this side of the planet. While the majority of respondents to our poll did – 64.5 per cent said yes, versus 35.5 per cent saying no – many of the resulting comments on the blog and on our Facebook Chat site were not so sure. It was not so much about whether a campaign would work, but whether we should even bother.
Many of the commenters, GPs and practice staff in the main, were of the opinion that faxes were entrenched in the healthcare system for very good reason: they are quick, easy, and everyone knows how to use them. Certainly there is a recognition that they were not exactly secure and there are plenty of GPs who detest them, but there are also plenty who say they are still the easiest, most reliable form of communication.

The Northern Territory government has launched an ambitious whole of territory digital strategy, backed by a digital stimulus package and underpinned by ongoing investments such as the $259 million core clinical systems renewal program (CCSRP) and a further expansion of the remote telecommunications co-investment program it runs with Telstra.
It also plans to commission a new government data centre at Millner, part of a data centre refresh works program that will relocate data centre services from the Chan building in Darwin CBD and establish a dual data centre model for government.

The initial findings from Australia's inaugural health information workforce census will be released at the HIMAA/NCCH conference in Hobart at the end of the month.
The census, a joint initiative between the University of Tasmania's Kerryn Butler-Henderson and the University of Melbourne's Kathleen Gray, is thought to be the largest of its kind in the world and is to replicated in New Zealand this year.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.