
Pulse+IT's weekly round-up of international health IT news for the week ending May 17: Kerala's corona slayer, Wales data hub, NHS tracing apps, AI for viewing scans remotely, FHIR-based data activation platform, EMRs for COVID research, FHIR in Russia, Google Nest for ward rounds, WHO app for underserved countries, swapping EMRs causes patient dissatisfaction
The coronavirus slayer! How Kerala's rock star health minister helped save it from Covid-19
The Guardian ~ Laura Spinney ~ 14/05/2020
KK Shailaja has been hailed as the reason a state of 35 million people has only lost four to the virus. Here’s how the former teacher did it

Much has been written in these pages and others about the way telehealth has fundamentally changed primary care during COVID-19, although whether that change will continue into the future is still a matter of debate. We are hearing more positive things about the Australian government's plans to continue with Medicare-funded telehealth after the pandemic, although our readers are hedging their bets on whether they think this will come to fruition.
We asked in our poll last week whether you expected to see MBS-funded telehealth continue after the pandemic. Lots of people doubt it, but a small majority is more positive, with 58 per cent saying yes and 42 per cent saying no. We are hearing that Health Minister Greg Hunt is keen, but the big sticking point for general practices in particular will be whether the items are required to be bulk-billed or not. If they are, we believe widespread provision of telehealth will prove financially unsustainable for general practices, and things will revert to business as usual.

Sydney Local Health District has massively ramped up its Royal Prince Alfred Virtual Hospital (rpavirtual) since the coronavirus pandemic began, rapidly redesigning its service to help manage 446 COVID-19 positive patients either at home or in special accommodation hotels since March.
rpavirtual has also seen a big increase in nursing and medical staff deployed to the service and a reconfiguration of its electronic medical record (eMR) to handle the crisis, while also capturing real-time data from wearable devices provided to patients.
The Institute of Environmental Science and Research (ESR) and health IT solutions vendor Sysmex have set up a national clinical data repository (CDR) for all COVID-19 test reports from testing labs across New Zealand.
The repository complements EpiSurv, the system ESR operates for the Ministry of Health on notifiable disease information from public health services.

Baxter Healthcare is providing its Sharesource remote patient management platform to Australian and New Zealand hospitals and dialysis clinics for free over the next six months for home-based peritoneal dialysis (PD) patients at high risk of COVID-19.
Sharesource technology is able to connect PD patients in the home with hospitals to allow health professionals to remotely monitor and adjust dialysis treatment.
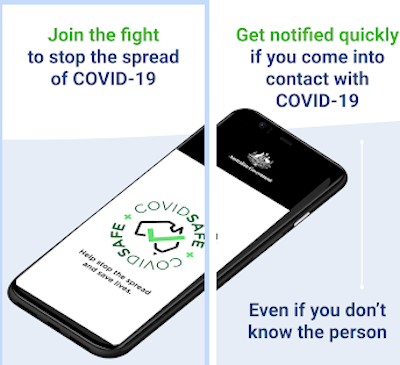
All Australian states and territories have signed on to use the COVIDSafe contact tracing app, which has now been downloaded by 5.6 million people.
Australia's deputy chief medical officer Paul Kelly said the app was now fully functional and the jurisdictions had all provided information on who in their public health units will be using it.

Pharmacy dispensing system vendor Minfos will release electronic prescription functionality free of charge to its 850 pharmacy customers from next month.
Pharmacists will be able to dispense ePrescriptions directly from Minfos Dispense without having to integrate with new software or significantly change existing dispensing workflow, the company said.

Melbourne's Austin Health has accelerated what was planned as a six-month roll-out of Microsoft Teams to help staff deal with the COVID-19 pandemic, managing to deploy it to support 8500 people in under two weeks.
Teams is being used by clinical and non-clinical staff for communication and collaboration, allowing multi-disciplinary teams meetings to be held despite isolation practices and for doctors to run virtual ward rounds.

Victoria's Northern Health is expanding its use of the Medtasker clinical communication and task management platform to 4G in addition to the onsite WiFi at its four facilities, allowing staff working in the community to receive and respond to tasks, including those caring for COVID-19 confirmed patients.
Medtasker CEO Paul Hirst said the pandemic had seen new functionality added to the platform as well as new uses for existing functionality. Medtasker can be used by all mobile hospital staff members, including doctors, nurses, allied health, pharmacists, cleaners, orderlies and security staff.

A consortium of Australian research groups is building a real-time clinical data and analytics platform (CDAP) that provides nationally available real-time analytics on the progression of COVID-19 to severe disease.
Funded by $4 million from the Digital Health Cooperative Research Centre, the data will be sourced from electronic case report forms, COVID-19 relevant EMR and GP data, third-party symptom tracking apps and electronic patient reported outcome data.
It will then be fed into a decision support tool based on Bayesian decision networks and returned to the clinician at the point of care through a web interface.

Pulse+IT's weekly round-up of international health IT news for the week ending May 10: Telehealth take-up, Canada invests in virtual health, NHS tracing app, Fitbit for aFib, patient matching problems, Apple heart study, FHIR boosts search in EMRs, spooks given access to NHS IT, contact tracing app analysis
Survey: More than 90% of physicians are treating patients remotely
MedCity News ~ Elise Reuter ~ 01/05/2020
Nearly half of physicians said they used telemedicine for the first time for a physical consultation.
Canada invests in virtual care, mental health tools
Canadian Healthcare Technology ~ Staff writer ~ 06/05/2020
Prime Minister Justin Trudeau announced an investment of $240.5 million to develop, expand, and launch virtual care and mental health tools to support Canadians.

There was good news for telehealth fans this week with new data about take-up in general practice and acute care emerging, topped off by Australian Health Minister Greg Hunt dangling the potential of a permanent role for publicly funded telehealth in the post-pandemic future.
A spokesperson for the minister told the Sydney Morning Herald this week that he had been lobbying for telehealth to continue after the pandemic. Considering Greg is in the position of actually being able to do something about it, we hope he does more than just lobby.
The new data from Melbourne's Outcome Health POLAR research backs up the anecdotal evidence that most telehealth consultations are being done by the phone, although the numbers the data has revealed are stark. Of the remote consultations conducted since mid-March by 1000 practices in NSW and Victoria, just five per cent are being done video, or just two per cent of overall consultations. People are still turning up to see their doctor in substantial numbers – POLAR's figures show 60 per cent of consults are still being done face-to-face – which might have something to do with people coming in for flu shots. The data is also showing that orders for pathology and radiology tests are way down.

Microsoft has announced plans to establish its first data centre region in New Zealand, saying it was a step toward delivering enterprise-grade cloud services in the country.
The New Zealand region will be the latest addition to Microsoft’s global footprint, with 60 regions in total. Its Azure cloud platform is now available in over 140 countries around the world.

Australia's first fully electronic prescription has been successfully prescribed and dispensed by a doctor and pharmacist in the Victorian town of Anglesea, using the token model developed by industry and regulators as an alternative to paper scripts.
The successful exchange was achieved using the Best Practice prescribing system, prescription exchange service eRx Script Exchange, Fred NXT Dispense and MedView Flow, a desktop tool that gives pharmacists a consolidated view of their medications workflow.

Melbourne's Royal Children’s Hospital is now delivering almost 70 per cent of its specialist clinic appointments by telehealth, with the average of 1200 face-to-face appointments per day dropping to 250 during the coronavirus pandemic.
RCH, which uses Healthdirect Australia's Video Call service for video conferencing, has been providing telehealth services to children living in rural and regional Victoria for more than eight years.

Eastern Melbourne Primary Health Network (EMPHN) has appointed former Telstra Health staffer Janine Wilson as CEO, taking over from Robin Whyte.
Ms Wilson was head of national registries at Telstra Health, managing the National Cancer Screening Register, and previously spent 11 years at the Australian Red Cross Blood Service.

The federal Department of Health is allowing aged and community care providers to use any unspent Commonwealth Home Support Program (CHSP) funds to buy up to $1000 of personal monitoring technology for vulnerable clients during the COVID-19 pandemic.
Older people receiving home care packages can also use their packages to access monitoring services, including to purchase suitable digital technology and video conferencing equipment and access assistance in setting up and learning how to use the technology.

A consortium of health and social care providers are working together on a trial of tailored digital health and wellbeing packages sent via SMS to people at risk of or experiencing homelessness, with a specific COVID-19 information package developed to support them during the pandemic.
The digital health toolkits have been developed to address five priority health areas including mental health, infectious disease, oral health, chronic disease and alcohol and other drugs, and will be sent to each person's mobile phone by their outreach worker using patient education specialist Healthily's GoShare platform.

Data gathered from 1000 general practices in NSW and Victoria using Outcome Health's POLAR GP data analytics tool has revealed that only a fraction of consultations delivered by telehealth during the COVID-19 crisis is conducted by video conferencing.
The most recent data shows that face-to-face consultations still make up 60 per cent of volume, and of the 40 per cent delivered by telehealth, only five per cent used video, with GPs far preferring telephone consults.

Online directory and appointment booking platform 1st Group has launched a new directory service allowing patients to search for telehealth providers and COVID-19 clinics, along with a secure telehealth solution that is fully integrated with its platforms and third-party practice management systems.
The new TelehealthClinics.com.au functionality is powered by the company's MyHealth1st directory platform and allows patients to search for GPs, dentists, pharmacists and a range of allied health providers such as psychologists in their local area. It will shortly also add search functionality on a nationwide basis no matter what telehealth system is being used by the provider or their location.

Cloud-based clinical and practice management system vendor MediRecords has partnered with Propell Health, the Australian distributor of the iHealth range of mobile health devices, to launch a remote monitoring solution aimed at chronic disease home monitoring, hospital in the home and remote care in residential aged care facilities.
Using iHealth's TGA-approved wireless devices, patients will be able to take their own blood pressure, glucose levels, pulse rate, oxygen saturation levels and weight readings.

Medicare billing app vendor Synapse Medical Services has partnered with virtual GP clinic Phenix Health to provide a mobile telehealth and billing solution for the COVID-19 pandemic.
Doctors can complete a telehealth consult on the Phenix platform, bill it, and receive a response from Medicare instantly to their phone along with overnight payment.

The Australian Digital Health Agency (ADHA) is offering up to $50,000 to digital health software vendors to come up with digital health solutions focused on clinical care, social care and enhancing national emergency preparedness infrastructure.
The offer is aimed at existing companies that can roll out the potential solution in the 2020/21 fiscal year and can offer rapidly designed, interoperable, safe and secure digital health services and technologies for both patients and providers affected by COVID-19.

Pulse+IT's weekly round-up of international health IT news for the week ending May 3: HIPAA future after COVID, EMRs and pandemic, NHS contact tracing app plans, COVID skills on Alexa, FHIR use cases, audio-only telehealth, extra info on Summary Care Record, de-identified data for COVID research, free telehealth of US uninsured, telemedicine kiosks in aged care
As coronavirus strikes, crucial data in electronic health records hard to harvest
Kaiser Health news ~ Fred Schulte ~ 30/04/2020
Over the past decade, federal officials have spent some $36 billion switching from paper to electronic health records, or EHRs, expecting, among other things, to harness volumes of medical data to reveal which treatments work best.
Will Covid-19 kill HIPAA? No, but…
MedCity News ~ Arundhati Parmar ~ 27/04/2020
Doctors, lawyers, data privacy and security experts weigh in on the future of HIPAA after rules have been relaxed to better tackle the public health crisis that Covid-19 represents.

It has become a cliché in hurry in these unprecedented times but the speed with which the health IT sector has had to adapt to the global pandemic has been stunning to watch. Healthcare usually changes at a snail's pace, for good reason, and health IT is no different. We asked in our poll last week if you thought the health IT industry has successfully risen to the challenge of COVID-19. Not surprisingly, the sector was positive about itself: 79 per cent said yes, 21 per cent said no.
And just as the dealing with a crisis playbook has been thrown out the window, so has years of recalcitrance on the part of the healthcare system and its policy designers in taking up new and not so new technologies. It took a global pandemic to finally get telehealth on the front foot and everyone is doing it now. It has been quite stunning to see how fast the local industry has been in developing solutions for users, with a plethora of video conferencing solutions now available.

IBM Watson Health has integrated its Micromedex reference database for medication information with EBSCO's DynaMed clinical content system to create a single, global solution suite to bring together drug and disease content.
Called “DynaMed and Micromedex with Watson” or Dynamedex, the solution promises to provide a single source for evidence-based insights to help inform clinical decisions.

Victoria's Bendigo Health is rolling out a telemonitoring solution built on Siemens Healthineers' teamplay myCare Companion platform to care for suspected COVID-19 patients at home.
The solution, which includes symptom tracking and monitoring devices and which can alert clinicians that the patient is deteriorating, is also being deployed for people with chronic disease who are at high risk and residents of aged care facilities to try to avoid the need for hospital admission.

Melbourne's Parkville precinct will go live with its $124 million electronic medical record on August 8, having been forced to postpone the original May launch date due to the COVID-19 outbreak.
Melbourne Health, the Peter MacCallum Cancer Centre and the Royal Women’s Hospital are joining the Royal Children’s Hospital in using the EMR from US firm Epic. RCH went live in 2016 and its emergency department module is now in use at Royal Melbourne Hospital's ED.

Practice management software vendor Intrahealth has added a fully integrated telemedicine module into its system as part of its Virtual Care initiative, promising a wholly integrated video experience within existing workflows for clinicians.
Intrahealth, which counts users in New Zealand, Australia and Canada in its customer base, says it has put aside its technology roadmap in response to the COVID-19 pandemic.

The Aged Care Industry IT Council (ACIITC) will launch an in-depth survey this Friday that aims to create a baseline from which aged and community care providers can benchmark their digital capabilities.
The survey is part of the Capabilities in Aged and Community Care Readiness, an Evaluation of Innovation and Technology (CAREIT) project, which has been funded by the federal Department of Health.

Brisbane's Metro North Hospital and Health Service is hoping to shift 30 per cent of its outpatients clinics to virtual services as the pandemic continues, moving beyond traditional telehealth to a virtual care system that allows for the real-time exchange of information.
The HHS also developed its own tracing app for patients arriving in Australia with suspected coronavirus, a workforce attendance tracker to keep a handle on clinical staff, a screening outcome notification app to let patients know by text of a negative diagnosis, and it is even biofabricating its own protective equipment, with TGA approval for its 3D printed face masks.

Researchers from the University of Sydney have developed a free national text message support program for people with chronic respiratory diseases who are unable to access usual hospital rehabilitation and support programs due to the COVID-19 pandemic.
Patients simply need to text the word “lung” to a support phone number to access the program, or sign up through a weblink or QR code. It is available to all patients wth chronic respiratory disease such as emphysema, chronic bronchitis and asthma free of change nationally.
Online appointment booking system vendor HealthEngine has launched what it is calling an end-to-end telehealth service, providing a full suite of options including a integrated video conferencing system, partnerships with third-party telehealth providers for a 24/7 service, as well as the ability for practices to use consumer-grade video conferencing platforms and telephone appointments.
It has also added a telehealth search feature to its directory that allows patients to find, book, see and pay for telehealth appointments with either their regular provider or a new one. This includes MBS funded telehealth services as well as paid consultations, with patients able to pre-pay at the time of booking.
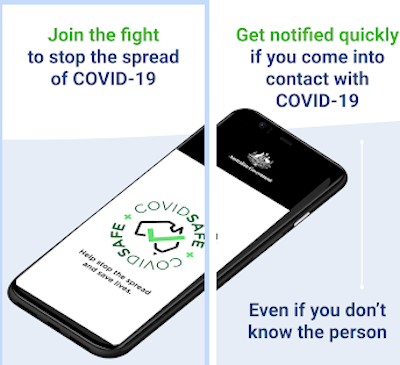
More than one million Australians have downloaded the COVIDSafe contact tracing app in its first day of release, part of the federal government's bid to automate and improve what state and territory health officials do manually.
The app uses Bluetooth to look for other devices that have the app installed and takes a note when that occurs, securely logging the other users’ encrypted reference code.

Pulse+IT's weekly round-up of international health IT news for the week ending April 26: 50% of US docs using telehealth, COVID-19 tracing apps, Epic supports interop rules, family pratices under threat, free devices for vulnerable Canadians, NHS app and pharmacies, DoD open to community health providers, Google Cloud Healthcare API, Fitbit to track COVID, patient portals
Half of physicians now using telehealth as COVID-19 changes practice operations
FierceHealthcare ~ Heather Landi ~ 23/04/2020
That's up from 18% of physicians using telemedicine two years ago, based on The Physicians Foundation’s "2018 Survey of America's Physicians."
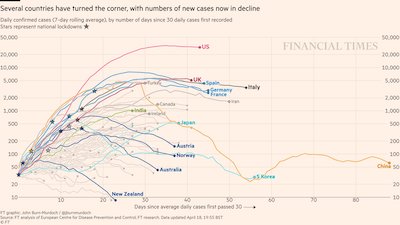
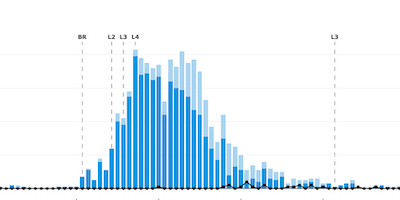
If like Pulse+IT these days you are getting your jollies hunting down maps and graphs of the coronavirus outbreak, you might have come across the great work being done by Financial Times data-visualisation journalist John Burn-Murdoch. Each day, he tweets out multiple visualisations of the pandemic and its growth in multiple countries, large and small.
He likes to keep his eye on the disasters in Italy, Spain, the UK and the US of course, but also regularly mentions certain countries that appear to have managed the outbreak pretty well, especially the ANNAs: Australia, New Zealand, Norway and Austria.

The four northern region DHBs are reporting good uptake by patients of appointments offered by video conference and telephone, with thousands of appointments going ahead that normally would have been cancelled during the COVID-19 lockdown.
The DHBs are using a variety of technologies for virtual appointments, including Facebook Live sessions for expectant parents and wide use of the DHB's Zoom telehealth system, which they began rolling out in 2018.

Queensland Health has terminated its $64 million laboratory information system replacement project, cancelling its contract with US vendor Sunquest and instead upgrading to the latest version of its existing Auslab system from Citadel Group.
Queensland Health has spent $37.5m so far on the project, more than half of the allocated budget, which was originally $68.5m when the tender was awarded to Sunquest in February 2018.

ASX-listed Oneview Healthcare has launched a cloud-based managed solution deployed on tablet devices that can be mounted on beds or rolling stands and lets clinicians conduct virtual rounds with patients and patients to call family and friends.
Called Oneview Cloud for COVID-19, the solution does not require integration with other systems and uses the hospital or aged care facility's own enterprise video applications such as Cisco Jabber or Microsoft Teams.

Patients attending Canberra Health Services (CHS) will be able to access some of their outpatients appointments by telehealth from next week with the roll out of Healthdirect's Video Call service.
Calvary Public Hospital Bruce appointments will follow for patients who may be self-isolating, in quarantine and those who are in high risk groups, such as elderly and immune suppressed people.

Melbourne-based patient engagement platform vendor HotDoc has been chosen by the Australian Department of Health to provide its appointment booking technology for the pop-up COVID-19 respiratory clinics that are being set up across the country.
HotDoc has already begun rolling out the software, which will help enable the federal government to widen the testing criteria for COVID-19 across Australia.

Hobart firm HealthCare Software (HCS) has won a contract with Ballarat Health Services (BHS) to roll out a clinical referral management system to allow tracking, triage and management of outpatient and clinic service referrals across multiple BHS facilities and specialties.
The solution will enable GPs, community healthcare professionals and Ballarat Health Service’s teams to seamlessly exchange patient information and referrals, replacing the current manual referral management process.

ACT Health director-general Michael De’Ath has stood down, effective immediately, and will return to Melbourne for family reasons, said to be in part due to the coronavirus pandemic.
Deputy director-general of health Kylie Jonasson has been appointed to the role of director-general for the next six months.

Patients in South Australia can register to receive negative COVID-19 test results faster from SA Pathology through a secure online platform developed in association with Adelaide digital health firm Personify Care.
The service provides patients with early notification of their test results being available and whether they need to continue to self-isolate. The full results will still be sent to the patient's nominated GP and be uploaded to the My Health Record.

Telehealth software developer Coviu has partnered with digital health start-up Rosemary Health to develop an integrated solution that will allow GPs and specialists to send a digital prescription to the patient’s pharmacy during a telehealth consult, and to arrange for the medications to be dispensed and delivered to the patient at home.
Originally conceptualised during the summer bushfire crisis, the partnership has been kickstarted by the coronavirus pandemic and the recent loosening of regulations for electronic and digital scripts.

Patients in regional areas of Victoria with ischaemic stroke are now receiving care that is comparable to metropolitan areas since the roll out of the Victorian Stroke Telemedicine (VST) program at 16 hospitals, new research has found.
The VST program provides clinical staff in regional emergency departments with audio-visual consultations with stroke specialists in Melbourne using a dedicated phone line and a telemedicine cart at the patient's bedside.




HotHealth forms and surveys
Patient engagement software vendor HotHealth has added new forms and surveys functionality to its platform, which enables healthcare providers to digitally communicate with clients and patients through video conferencing, community engagement tools and online bookings.
The online forms function can help screen high-risk clients prior to consultations and provide an alternative to face-to-face appointments, HotHealth says.
It will also allow patients to register via an online patient registration service, completing their own demographic details and providing telehealth consent, all of which can be automatically sent to the practice system.
It also has a drag and drop form builder to create custom forms specific to each organisation’s requirements, but there are also pre-made template available for organisations to use or start from.
Examples include patient registrations forms, COVID-19 screening forms, referral requests and feedback surveys all of which are accessible via a link, SMS, mobile phone, tablet or desktop.
PPMP
Practice management software vendor PPMP has added an option to conduct telehealth appointments through its online booking system.
Practices wanting to access the functionality need to have the PPMP online booking system. Those that do can now access Zoom for video conferencing and Stripe for payments.
Genie Solutions
Genie Solutions says its practice management platform, including its Genie desktop and Gentu cloud offerings, is providing tools to help meet the changing requirements of practices and their patients during the crisis.

Digital Health Guide
The team behind the Digital Health Guide has added new resources to its platform specifically for the COVID-19 pandemic, in addition to the hundreds of existing resources it already covers. These include apps and web-based solutions relating to mental health and physical activity, which will be useful for people dealing with the mental health effects of self-isolation and quarantine.


Pharmacists and telehealth
The Pharmaceutical Society of Australia (PSA) has provided guidance on the regulatory changes recently made that allow for digital prescriptions in each state and territory. It has also developed some resources in association with the Australian Department of Health on using telehealth for home medicines reviews and residential medication management reviews.
This includes guidance on the workflows involved in using audio and video technology, the common consumer applications, how to book a consultation and what to do during the consultation. There is also a leaflet on digital devices that pharmacists can recommend to patients and a detailed leaflet to give to patients that explains what telehealth is and what to expect in a consult.

MBS item numbers
The Australian Department of Health has released the new item numbers for bulk-billed telehealth consultations and pathology services. Details are available here. PMS vendors are now implementing the new numbers in their software.


Community pharmacists will be allowed to deliver home medicines reviews and aged care residential medication management reviews by telehealth from tomorrow in a temporary move during the coronavirus pandemic.
The changes also allow them to provide MedsChecks and Diabetes MedsChecks by telehealth to eligible patients, which normally involves face to face consultations in the pharmacy to help patients with self-management and to identify medication-related problems such as non-adherence.

Clinical software vendor Genie Solutions will this week roll out the first iteration of its new telehealth solution TeleConsult, powered by Amazon Chime, one of four products on its new platform that aims to provide an end-to-end telehealth workflow solution for medical specialists.
The company is also set to release a booking system with triage capabilities it has been developing with online appointments specialist HotDoc, along with a new online payment system it has developed with Ezidebit and an online patient registration service that lets new patients register their demographic details.

Pulse+IT's weekly round-up of international health IT news for the week ending April 19: Covid-19 effect on UK primary care, Canada pays EMR vendors to upscale, vendor-agnostic ICU solution for Covid-19, teledentistry, malware trifecta, Tricorder app, virus boost for telehealth uptake, aged care links to ED by VC, Attend Anywhere rapid deployment, consumers keen on virtual care, everyone is building contact tracing apps
The month primary care went remote due to Covid-19
Digital Health News ~ Jon Hoeksma ~ 15/04/2020
The Covid-19 crisis has, in a few short weeks, led to the most dramatic transformation of primary care services ever seen, with most consultations moved to remote and virtual to comply with social distancing.
Virtual acceleration program for EMR vendors
Canadian Healthcare Technology ~ Staff writer ~ 15/04/2020
The Infoway EMR-Virtual Care Investment initiative will provide participating EMR vendors with financial support to rapidly integrate or scale existing virtual care technologies to meet the growing demand during the pandemic when Canadians are encouraged to observe physical distancing.

Pulse+IT had a bit of a dig at the announcement a month or so ago by Australia's Department of Health that it would pull off a ”development sprint” over eight weeks to get electronic prescriptions happening in the face of the pandemic.
We were highly cynical that it could be achieved in such a timeframe (and for just $5 million), but we might be laughing on the other side of our smug face soon enough as the GP software vendors seem to have pulled off the miraculous and are now on track to make the capability available next month at the earliest.

GP clinical software market leader Best Practice Software has completed development work to enable electronic prescriptions and has begun its testing phase, targeting mid-May for the first release of the functionality.
Zedmed is also hoping for a mid-May switch-on date and other vendors such as Medtech Global, MediRecords and MedicalDirector are also working on the capability, with Medtech and MediRecords aiming for a June or July roll out while MedicalDirector said it was working towards the Australian Digital Health Agency's timelines.

The Western Australian and Australian Capital Territory primary health networks are partnering with Healthdirect Australia to provide its Video Call telehealth service free of charge to medical practices in their catchments to assist with the coronavirus pandemic.
The WA Primary Health Alliance (WAPHA), which manages the two Perth PHNs and Country WA PHN, launched the service last week, with 100 practices enrolling.

ASX-listed respiratory health monitoring platform Respiri has partnered with Phenix Health to integrate its Wheezo app with Phenix Health's telehealth platform, patient dashboards and asthma management plans.
Respiri, formerly known as iSonea, produces digital wheeze detection and measurement technology that can record airway sounds to and measure the extent of wheezing caused by airway obstruction.

New Zealand's leading pharmacy and general practice software vendors have come together to launch an integrated electronic prescription messaging service called Secure Script that will allow GPs to send signature exempt eScripts directly to pharmacies.
Pharmacy platform RxOne and GP practice management software vendors Indici and My Practice rolled out the capability in their respective systems last month, using secure messaging service Clanwilliam Health (formerly HealthLink), and they have now been joined by the market-leading pharmacy dispense and GP PMS vendors, Toniq and Medtech.
And in another breakthrough for ePrescribing in New Zealand, Waitemata, Auckland and Counties Manukau District Health Boards have announced they will start using Secure Script in the near future.

Patients in Western Sydney who have contracted the coronavirus but are at low to medium risk of serious illness are being remotely monitored at home by GPs and hospital-based community health teams using CareMonitor's shared care software and biometric measurements such as temperature, oxygen saturation, blood pressure and heart rate.
COVID-19 positive patients presenting at Western Sydney Local Health District hospitals are being triaged using a risk assessment protocol in CareMonitor and based on the risk severity rating, are being referred to GPs to be managed in the community.

Apple and Google have announced a joint effort to use Bluetooth technology to help reduce the spread of the coronavirus through a contact tracing platform.
In a two-part roll-out, the technology giants will release application programming interfaces (APIs) next month that will enable interoperability between Android and iOS devices using apps from public health authorities. These will be available for download via the respective app stores and only public health authorities will be allowed to use them.

Patients in NSW are being given the opportunity to receive their COVID-19 pathology results on the same day via text message in a collaboration between NSW Health Pathology, Amazon Web Services, Deloitte Australia and Microsoft.
The automated SMS solution has been trialled in the Illawarra Shoalhaven Local Health District and Wollongong, Shellharbour and Shoalhaven fever clinics and will be rolled out to other NSW facilities in the next few weeks. Western Australia introduced a similar service last month.
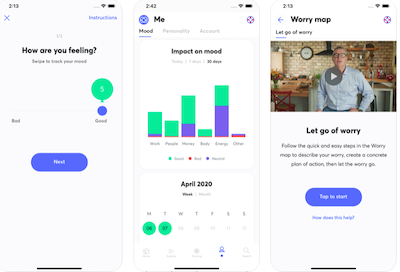
The New Zealand government is funding three mental health resources to help people look after their wellbeing during the coronavirus pandemic, including an app developed by rugby player John Kirwan that provides tips and techniques for dealing with anxiety, the health journal app Melon, and a cognitive behaviour therapy tool called Staying on Track.
Access to the apps is being funded as part of the government's $NZ500 million COVID-19 response health package, and a version of the Melon app specifically for 13 to 24 year-olds is being developed now.

Pulse+IT's weekly round-up of international health IT news for the week ending April 12: Formulary of COVID apps, pandemics and privacy, Bahrain tracks with electronic bracelets, dashboard to track pandemic equipment needs, telehealth in the long term, NHS Teams, more Zoom vulnerabilities, COVID-19 data platform, US consumer views on telehealth
ORCHA launches library of clinically approved Covid-19 health apps
Digital Health News ~ Andrea Downey ~ 08/04/2020
App evaluation company ORCHA has launched a Covid-19 formulary to signpost healthcare professionals and consumers to clinically validated apps.
COVID-19 pandemic opens up new frontiers for health data privacy
Healthcare IT News ~ Piers Ford ~ 08/04/2020
While European governments look to digital health technology for ways to speed up their containment strategies, the long-term view is that the COVID-19 emergency will generate new approaches to sharing healthcare data once the pandemic has passed.

Clinical and practice management software vendor MedicalDirector has launched an integrated telehealth capability in its cloud-based Helix system, with similar functionality to be made available in MedicalDirector Clinical in the near future.
Patients will be sent a secure link prior to their appointment and the GP simply needs to launch a telehealth consultation from within the patient's record. The patient's notes and history are displayed in a window alongside the video stream and GPs can update the record during the consult.

Eye health clinical communications network Oculo will shortly launch video conferencing technology in its platform to support teleophthalmology and teleoptometry.
Oculo users will be able to conduct teleconsultations directly from the Oculo platform, which can be used as a standalone system but is also integrated with some electronic medical records and with Topcon's Harmony image management system.

Cloud-based medical and allied health practice software vendor Mediclinic has added icons to its diary and booking page to allow practitioners to call or video conference with patients using common consumer apps such as Skype, WhatsApp, FaceTime and Viber.
Mediclinic, which is predominantly aimed at allied health and medical specialist practices but is also available for the GP market, is currently developing an in-built WebRTC-based capability that will automatically record all conversations to the patient file. The video itself will not be recorded.

The NSW Ministry of Health has partnered with patient education specialist Healthily to enable digital information packages on COVID-19 to be sent to patients by SMS from 51 NSW emergency departments and COVID clinics.
The multi-lingual packages will be sent through Healthily's GoShare patient education platform and will provide hospitals with access to three interactive information packages about prevention, symptoms and diagnosis of COVID-19.

Patient engagement platform HotDoc has released new payment functionality to its booking system that will allow clinics to apply their normal billing practices to telehealth appointments.
The Department of Health is now allowing practices to privately bill patients for telehealth appointments who don't fit the bulk-billing criteria.

The Australasian Institute of Digital Health (AIDH) is holding its inaugural virtual conference at the end of April, fittingly focusing on how telehealth is being deployed to fight the coronavirus pandemic by those on the frontlines.
The day-long conference will hear from Healthdirect CEO Karen Borg on Australia's telehealth response to COVID-19, along with Télémédecine 360 medical director Robin O’Hannessian on France's public health response and PinkTech Design CEO Kanav Kahol on India's experience.

ASX-listed software vendor the Citadel Group has completed the $200 million purchase of UK radiology and maternity software vendor Wellbeing Software Group.
Citadel announced its intention to buy Wellbeing in February with the aim of cross-selling its pathology and oncology solutions into the UK and bringing Wellbeing’s offerings into the Australian market.

Townsville Hospital has reinstalled the WinChart anaesthetic solution from Getz Clinical on the insistence of its anaesthetists, who campaigned for several years to keep the solution rather than swap to the anaesthesia module in the state's integrated electronic medical record (ieMR).
WinChart has been used for many years in Queensland, first rolling out at Cairns Hospital in 2008 as part of the Automated Anaesthetic Record Keeping (AARK) program before being implemented at the majority of the tertiary hospitals in the state.

Real-time remote monitoring and shared care platform CareMonitor has gone live with a new telehealth system that users can access through Pen CS's Topbar app.
CareMonitor CEO Deepak Biswal said that while the platform already had the ability to do video consultations in its core shared care management product, the new offering was a standalone telehealth solution that can be used by any healthcare provider. The platform has been specifically optimised for remote consultations, triaging and fever clinics.

ASX-listed ResApp Health will partner with Brisbane-headquartered telehealth provider Phenix Health to integrate ResApp’s acute respiratory diagnostic test into Phenix’s telehealth app.
ResApp has recently completed a similar integration of ResAppDx-EU into Coviu’s telehealth platform and is expecting to have it available for use in a few months. The company is also about to launch a consumer-focused smartphone app for sleep apnoea.
Pulse+IT's weekly round-up of international health IT news for the week ending April 5: Barts builds digital hospital in one week, $200m for US telehealth, wearables time has come in EU, privacy relaxed for COVID-19, vulnerabilities in Zoom VC, digital passport for credentials, NHS fast-tracks digital tool for GPs, virtual meds reconciliation
Barts extends Cerner EPR to NHS Nightingale hospital
Digital Health News ~ Owen Hughes ~ 31/03/2020
Remarkably, the huge IT project has been achieved in less than a week, with the Barts Health team led by CIO Sarah Jensen.
FCC proposes $200M telehealth program to tackle Covid-19
MedCity News ~ Elise Reuter ~ 31/03/2020
Federal Communications Commission Chairman Ajit Pai rolled out plans for a $200 million fund to help healthcare providers purchase telehealth tools to handle Covid-19.

After the virus, are we ever going back? We've been chatting to a number of experts in the field of telehealth this week and the consensus seems to be that now that the dam has broken, it is highly unlikely that we will revert to business as usual after the pandemic is over. Healthcare professionals will see that it is not always necessary for patients to present themselves in person, and we live in hope that funders like Medicare will no longer fear that the system will be rorted and instead embrace the savings and quality of care that can be achieved.
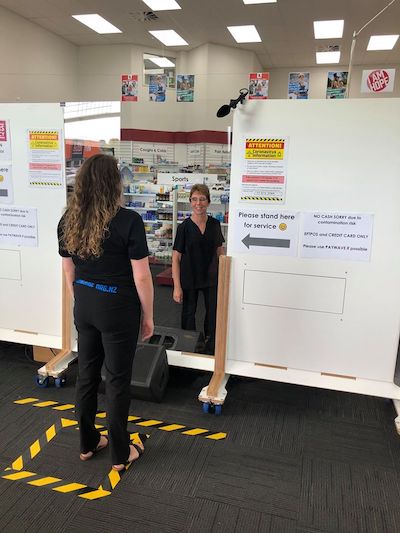
We are closely watching how things are panning out for the healthcare system in locked-down New Zealand, where some general practices simply will not see a patient unless they have been triaged by phone first. Hospitals are doing that for outpatients too, telling patients not to present unless specifically asked to. One DHB has even launched a fundraiser to buy remote monitoring devices for chronically ill patients to try to keep them at home. As Australia's CSIRO showed four years ago, widespread remote monitoring could save billions every year if fully embraced. Now would seem the time to seriously consider it. Things have changed utterly and we don't think they'll ever go back.

EMR vendor Allscripts has released a user-agnostic digital triage solution for emergency departments in Australia and New Zealand to help them cope with the demands of the COVID-19 pandemic.
Called Virtual Triage, the solution can be implemented in a matter of days at any healthcare site regardless of the EMR deployed and does not require patients to be pre-registered with the particular healthcare site, Allscripts says.

Several of Australia's private health insurers have agreed to cover tele-physiotherapy consultations for members during the COVID-19 pandemic, along with telehealth consults with psychologists.
The health funds will make the cover available from April 14 for remote consultations for orthopaedic surgery rehabilitation, cardiac rehab, pulmonary rehab, pelvic floor muscle training and for chronic musculoskeletal conditions such as osteoarthritis.

Waitematā District Health Board's charity arm the Well Foundation has launched a new charitable initiative to provide patients with serious health conditions with remote monitoring technology to reduce their need to visit hospital and potentially expose themselves to the coronavirus.
The program could see up to 100 patients with long-term health issues such as diabetes, respiratory and heart conditions receive equipment to monitor their heart rate, blood pressure, temperature and blood oxygen level at home. They will be shown how to enter their data into mobile devices to be shared with and monitored remotely by their hospital care team.

Melbourne-based Global Health has joined the Bp partner network as an approved integrator with Best Practice Software.
The agreement covers Global Health’s ReferralNet secure messaging system, which has been integrated with Bp Premier for a number of years and is also fully interoperable with Telstra Health's Argus secure messaging system, and Global Health's new HotHealth telehealth platform.

ASX-listed medications adherence software vendor MedAdvisor is bringing forward the planned launch of its medications home delivery service due to the COVID-19 pandemic.
The ASX-listed company announced last year that it had signed an agreement with transport and logistics provider Kings Transport to enable pharmacies to offer medication delivery to their patients.

Several Queensland primary health networks (PHNs) are working with general practices in their regions to send interactive COVID-19 information packages to high-risk patients using the GoShare Plus platform.
The information packages are available in 10 languages and are informed by Australian Department of Health and World Health Organisation guidelines. They include three consumer-reviewed digital information packages that have been developed by patient education specialist Healthily, providing critical information on prevention, symptoms and diagnosis of COVID-19.

Queensland Health has increased the capacity of its telehealth services to handle up to 1600 users at a time to try to help ease the burden on the state's health system by offering more remote consults with patients at home.
eHealth Queensland has also boosted the number of users who can now work from home and access all their existing corporate and clinical applications up to a capacity of 48,000.

Northland District Health Board has partnered with Clanwilliam Health to build an integration into Whangarei Hospital's clinical platform to enable electronic referrals to be sent between hospital departments and out to private specialists and community providers.
GPs have been electronically referring into hospitals in the region since 2013 using Clanwilliam Health (formerly HealthLink) technology but referrals between hospital departments have remained paper-based until the beginning of this year.

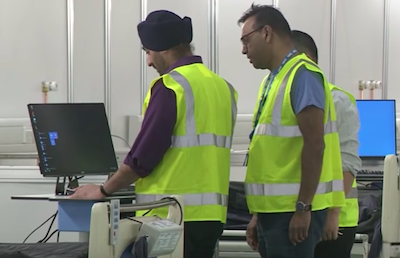
InterSystems has worked with five clinical laboratories to fast-track the development of a new interface between its TrakCare laboratory information system and PCR analysers being used to test for COVID-19.
The interfaces are allowing for faster turnaround times for test results and in the case of Sydney's Austech Medical Laboratories, will allow it to set up a specialised PCR lab that aims to help reduce the load on public hospitals and support home visits for patients unable to attend a medical centre.

A team of Australian software developers has come up with an open source approach to help medical practices handle patient arrivals and infection control during the coronavirus outbreak, working to turn around a minimum viable product in less than two weeks.
Dubbed Clinic Arrivals, the solution is a mixture of open source video conferencing, SMS messaging and integration with practice management system appointment books to manage telehealth consults and to automate the process of instructing patients what to do when they arrive for a face-to-face visit.

The federal government has doubled the bulk billing incentive from today as part of its expansion of Medicare-subsidised telehealth during the coronavirus pandemic.
There are now individual MBS items covering GP services and some consultations provided by specialists and nurse practitioners for video conferencing and for telephone consultations if video is not available. Doctors are also allowed to mail or email a prescription to the patient or the patient’s pharmacist.

Pulse+IT's weekly round-up of international health IT news for the week ending March 29: Sharing PHI in a pandemic, COVID-19 health IT coalition, NHS video consult panel, EMR strengths/weaknesses, AI success exaggerated, real-time location apps and coronavirus, Fitbit to track virus, COVID-19 hackers and spoofers
HHS: Information on COVID-19 patients can be shared to protect first responders from infection
FierceHealthcare ~ Heather Landi ~ 25/03/2020
Healthcare providers can share COVID-19 patients' medical information without their express authorization to help protect first responders from the risk of infection, the Department of Health and Human Services (HHS) said.
Health IT heavy-hitters join forces for COVID-19 Healthcare Coalition
Healthcare IT News ~ Mike Miliard ~ 24/03/2020
The private-sector collaborative includes EHR vendors (Epic, athenahealth), Big Tech (AWS, Microsoft), health systems (Mayo, Intermountain) and others, all working to speed development of "secure, ethical, innovative, open source" tools.

The quick response from the health IT sector in Australia and New Zealand to the coronavirus pandemic has been pretty impressive, with software vendors rolling out COVID-19-specific applications at a rate of knots if our technology resources page page is anything to go by.
Vendors are either tailoring new functionality to help with the crisis or in some cases waiving fees to ensure the technology is used when it's needed. An example is online appointment booking service Healthsite, which has very quickly managed to roll out a complete telehealth solution, in association with Tasmanian telehealth provider GP2U, that is integrated with Healthsite's booking system. HealthEngine also provides a similar service and both allow practices to offer private billing as well as bulk billed consultations.

The Victorian Department of Health and Human Services will use the Whispir cloud-based communications platform to keep in contact with the estimated 1700 people who are in self-isolation having been in close contact with a person diagnosed with COVID-19.
DHHS will use the Whispir platform to send interactive two-way messages and real-time updates to sufferers and those who have been in close contact with COVID-19 as part of its coronavirus containment plan.

The Australian Digital Health Agency has reopened its mobile gateway to developers looking to connect to the My Health Record through mobile apps.
The agency temporarily closed down the gateway to new entrants in 2018 while it undertook a privacy and security review, allowing only four apps to remain connected. They are Telstra Health's HealthNow, Chamonix's Healthi, and HealthEngine. The fourth app, Tyde, is no longer in business. Consumers can also access their record through myGov.

Healthsite is now offering practices a comprehensive telehealth solution that is fully integrated with its online booking system, using WebRTC technology adapted by telehealth specialist GP2U.
The solution will allow practices to offer both bulk-billed and privately billed telehealth consults with a secure online payment facility and instructions for both patient and doctor about the steps to start the consultation.

Melbourne Health has postponed the go-live of the $124 million Epic electronic medical record at the Parkville precinct due to COVID-19.
The precinct, which includes the Royal Melbourne Hospital, the Royal Women's Hospital and the Peter MacCallum Cancer Centre, was due to go live in May after a two-year implementation project.

The HealthPathways community has over the last two weeks put its exclusive focus on developing and maintaining local pathways for the COVID-19 pandemic and adapting national and state emergency response plans and clinical guidance for general practice teams.
The platform is an online manual used by clinicians in New Zealand, Australia and the UK to help make assessment, management and specialist request decisions for over 550 conditions. Each health jurisdiction tailors the content of HealthPathways in the local context.

Last week, the Australian government announced a $444.6 million package for the aged care sector to ensure the continuity of the aged care workforce, $92m of which will go towards additional support for home care providers and organisations that deliver the Commonwealth Home Support Program (CHSP).
There is also $78.3m for residential care to support continuity of workforce supply, and $234.9m for a COVID-19 retention bonus to ensure the continuity of the workforce for staff in both residential and home care.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.