
As the second year of the COVID-19 pandemic began to wind down and vaccination rates shot up, technologies to support the removal of restrictions on movement came to the fore. Vaccine certificates from the Australian Immunisation Register (AIR) were made available through the Medicare Express Plus app and MyGov and could be stored in digital wallets, but concerns over the ability to fake the certificates began to rise.
The states and territories were taking their own road for vaccination passes, with NSW beginning a trial of a state-wide solution linking the certificates to the NSW government’s Service NSW app. Others were working to add COVID vaccination certificates to each jurisdiction’s check-in apps, with the federal government saying this approach was necessary as public health orders and check-in QR codes are controlled by the states.

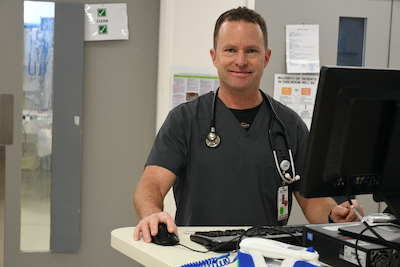
The rise of virtual care was undoubtedly the feature of 2021 in digital health, but it was in the more mundane and yet essential area of online appointment booking and patient management solutions that characterised the third quarter of the year in Australian and New Zealand eHealth. Both countries experienced delays in rolling out technology to manage vaccination bookings that we believe should have been solved in 2020, when it became clear that a global mass vaccination effort was the only way to manage it.
While booking systems were rolled out just in time, but it seems that at the end of 2021, more work still needs to be done. Just this week, HotDoc was adding Pfizer bookings for five to 11-year-olds across Australia and all services were working hard to add slots for booster shots to their systems. It’s pretty clear that we will have to live with the novel coronavirus as new infections rise across an increasingly jaded global populace, not defeat it. Omicron may not be as severe as delta, but it appears we will all get a bit more familiar with the Greek alphabet as we move into the new year.
Innovative solutions to help with the COVID-19 vaccination program continued to come thick and fast as we entered the second quarter of the year, and few were bigger than ACT Health’s solution. It went live with a full version of its new Epic EMR 18 months earlier than scheduled to help manage COVID-19 vaccinations for the ACT public health system.
While a full version of the EMR hosted on infrastructure provided by NTT is live, ACT Health only configured those parts of Epic required to manage the vaccine program as well as an online booking system using Epic’s MyChart patient portal, which has been branded as MyDHR (digital health record). Nursing staff administering the vaccines used Epic’s Rover smartphone app on Spectralink Versity handsets, with data from Epic and the territory’s iPM patient administration system then uploaded to the Australian Immunisation Register. The booking system for the ACT’s two COVID-19 mass vaccination clinics was up and running in May.

The 2021 Australian eHealth year in review was, as expected, dominated by news relating to the COVID-19 pandemic, but there were a host of topics of interest in the first quarter of the year, including online appointment booking systems, the embrace of telehealth and remote monitoring, progress in real-time prescription monitoring, and a number of big-ticked announcements with electronic medical record implementations.
The year kicked off with a new face at the Australian Digital Health Agency (ADHA), with former Queensland Health chief health information officer and Mater Health CIO Mal Thatcher named as the agency’s new chief technology officer (CTO). Taking over from former CIO Ronan O’Connor, Dr Thatcher is in charge of system operations including cyber security, core systems testing services and operational events.

10 years of FHIR, criteria-led discharge pathways, hospital builds its own EMR, patients wary of privacy in virtual health, doctors wary of wearables, telehealth access for America campaign, medical device security
HL7 celebrates 10 years of FHIR health IT data standard
EHR Intelligence ~ Hannah Nelson ~ 09/12/2021
As the health IT data standard matures, HL7 officials said that the organization plans to put out FHIR Release 5 in 2022.

This week saw international standards body HL7 celebrate the 10th anniversary of the adoption of the FHIR specification, which has since become one of most widely used standards in the world for healthcare interoperability. Created by Victorian Grahame Grieve and now adopted by any global health software company worth its salt, FHIR is widely touted as nothing short of a revolution in health IT.
We remember doing some of the first reporting on FHIR back in the early days, when we were alerted to the concept by former chair of HL7 Australia Klaus Veil. Klaus told us back in 2012 that FHIR was “the latest trending interoperability technology that has taken the eHealth world by storm”, and he was right. The promise was that it would be faster, easier and far more comprehensible than standards like HL7 v3, which got so bogged down in its own complexity that it was pretty much dropped.

As the second year of the COVID-19 pandemic began, the embrace of virtual healthcare provision continued to define this era in the eHealth sector. Telehealth, remote monitoring and electronic prescriptions saw notable developments, and yet it was the more prosaic field of online appointment booking systems and immunisation registers that defined the year in digital health.
The ramifications of the sweeping changes recommended by the Simpson Health and Disability System Review (HDSR) are still being debated but technology as an enabler of system reform will be front and centre, backed up by a pretty decent investment from the government in data and digital infrastructure of $400 million over four years.

It was the cybersecurity scare at Waikato DHB that dominated our most-read articles for the year, and the incident continued to make headlines in the following weeks and months. The saga of the build and roll out of the National Immunisation Solution was also top of mind, as was the controversy that followed it.
Medtech’s brand new Application Layer EXchange (ALEX) platform was also keenly watched as more vendors signed on. Medtech’s huge footprint in primary care in New Zealand means people sit up and take notice when it rolls out something as new – and potentially revolutionary – as this FHIR-based initiative, and our readership figures proved pertinent.

Auckland District Health Board will roll out the TrakCare patient administration system (PAS) from InterSystems, with the cloud-hosted solution set to begin implementation next month.
The solution will replace three patient management systems used by the DHB and will be used at Auckland City Hospital, Starship Children’s Hospital and multiple community organisations.


Melbourne’s Austin Health will be the first health service in the Asia Pacific region to implement Cerner’s Fast Health Interoperability Resources (FHIR) service, allowing it to access both Cerner and third-party SMART on FHIR apps as part of its interoperability strategy.
Austin Health is also taking advantage of Microsoft’s FHIR capabilities to exploit the capabilities of the Microsoft suite it uses, including Office 365, Azure and in another innovation for a health service, Microsoft’s Dynamics customer relationship management (CRM) platform.

Telstra Health’s primary and community care software system Communicare has integrated with the National Cancer Screening Register (NCSR), providing support for patient participation in both the cervical and the bowel cancer screening programs.
Communicare joins Best Practice and MedicalDirector in integrating with the NCSR. The system allows GPs and community healthcare providers to access their patients’ bowel and cervical cancer screening data and receive notifications of overdue screenings.
The developers of the $70 million Kaweka Health facility currently under construction in Hawke’s Bay have chosen the Get Well solution from ASX-listed Hills Health Solutions as its patient engagement platform.
Kaweka Health, which will open the first stage of the elective surgery facility in Hastings next year, is also planning to roll out Orion Health’s hospital information system as its EMR.

Loddon Mallee Health Network has rolled out a virtual home monitoring solution for low- and medium-risk COVID-19+ patients across 16 health services covering 25 per cent of regional Victoria, designing and implementing a module within its regional care coordination platform (RCP) in just two weeks.
The RCP uses DC2Vue home health monitoring technology from Melbourne’s Data Capture Experts, which has been previously rolled out to provide clinical assessments, coordination via web dashboards and integrations with hospital patient administration systems (PAS) to provide a high-end view of patients in the region. The COVID-19 solution is leveraging this existing technology and establishing a platform that can now be used for other conditions into the future.

The Digital Health Cooperative Research Centre (DHCRC) has launched a new project to improve medication selection and dosing for patients with poor kidney function, including a trial of how to incorporate it into primary care and community pharmacy settings.
The tool has been conceptualised as a standalone service that will be delivered via an application program interface (API) to allow for easy integration with existing prescribing and dispensing software systems.

Gippsland Primary Health Network is promoting a new positive pathway model of care for GPs to help them use existing technology to monitor low risk COVID+ patients at home.
Gippsland PHN has been supporting the LifeguardMobile platform from US firm Lifeguard Health Networks since last year, working with the Gippsland Region Public Health Unit (GRPHU) to roll out the technology, which includes a web portal and mobile app for health providers and a mobile app for patients that allows them to report their outcomes and vital signs.

Healthcare artificial intelligence vendor harrison.ai has raised $129 million in private equity to help develop its clinical AI applications, including investment from pathology giant Sonic Healthcare to help it pursue pathology AI solutions.
The company has an existing joint venture with medical imaging provider I-MED Radiology for annalise.ai, which is involves AI for clinical decision support for chest x-rays and is used by more than 350 radiologists each week.

Cross-border information sharing international patient summary, patient portals help early discharge, Ireland’s digital health plans, Zoom integration with Cerner EMR, digitising social care in the UK, talking prescription labels for visually impaired
In a boost to interoperability, SNOMED CT to power IPS sub-ontology
Healthcare IT News ~ Kat Jercich ~ 29/11/2021
SNOMED International says it will create and release an openly available International Patient Summary sub-ontology in the first half of 2022, aimed at promoting cross-border information sharing.
Patients with active patient portals get out of the hospital faster, Epic data shows
FierceHealthcare ~ Anastassia Gliadkovskaya ~ 29/11/2021
Patients with an active patient portal are more likely to have shorter hospital stays, according to a new study based on data from electronic health record giant Epic.

As the Omicron variant of the coronavirus plunges the world into new waves of restrictions and reinforces that COVID-19 is here to stay, governments around the world are struggling to communicate a long-term plan for living with the virus. This is most obvious in the public squabbles over vaccine mandates and passports, but also in shifting the burden from acute to primary care.
It is very clear that we will need to live with COVID-19 in the community for the foreseeable future, and we very much need to come up with long-term solutions on how to manage it as efficiently and financially sustainably as possible. The obvious answer is in technology solutions, of which there are many but which very much need to be backed up by long-term workforce reforms and needless to say, a bit of cash.

Ballarat Health Services (BHS) has expanded its existing BHS at Home model of care to roll out the cloud-based Patient Watch system to help monitor COVID-19 positive patients at home.
Patient Watch offers a lower cost model to other community-based remote monitoring services by allowing non-clinical staff to monitor patients, with a real-time clinical decision assistance engine called PaJR alerting them to escalate problems to clinical staff if they arise.

Sonic Pathology Australia chief medical officer Lawrie Bott has been appointed as the new president of the Royal College of Pathologists of Australasia (RCPA), succeeding Waikato DHB anatomical pathologist Michael Dray.
Dr Bott and Dr Dray served as RCPA vice president and president between 2019 and 2021, during what has been one of the most challenging periods for the pathology sector due to the COVID-19 pandemic.

Whanganui District Health Board (WDHB) has gone live with the Electronic Request Management System (ERMS) for eReferrals, the first North Island DHB to do so.
ERMS has been used by South Island GPs for more than a decade to pre-populate referral forms and deliver them to hospital departments and specialists.

Not-for-profit IT services organisation Patients First is closing down at the end of the year, transitioning control of its services to the New Zealand Ministry of Health.
Patients First was set up over a decade ago to provide a number of interoperability services, most notably the GP2GP electronic medical record transfer system.
GP2GP went live in 2012 and is a standards-based approach to transfer medical records between different practice management systems (PMS) when patients change practices.

Australia’s Minister for Health Greg Hunt is strongly rumoured to be retiring from politics at the next election, with insiders saying he is tipped to quit on Thursday, the last sitting day of Parliament for the year.
Mr Hunt, who was appointed minister of health in January 2017, is also minister for aged care. He was previously minister for the environment.

The Australasian Institute of Digital Health (AIDH) has launched a new leadership program for women working in the digital health field, offering a six-month program to help women develop their leadership potential.
The program is similar to one developed by AIDH board member and director of the Centre for Digital Health Transformation at the University of Melbourne, Wendy Chapman, in the US.

Melbourne’s Cabrini Health and The Alfred have gone live with the cloud-based ZEDOC platform from Auckland-headquartered The Clinician to automate the collection and analysis of patient-reported outcome measures (PROMs) for patients with colorectal cancer undergoing surgical treatment.
The project has enrolled 40 patients so far and is aimed at understanding both the health-related effects of cancer treatment on quality of life as well as supporting clinical teams to deliver more personalised care.

New Zealand’s opposition National Party is being led by Whangarei GP Shane Reti for the next week after leader Judith Collins was dumped in a party room vote of no confidence on the weekend.
Dr Reti, National’s deputy leader and health spokesperson, has an interest in health IT and completed a Harkness fellowship at Harvard Medical School on patient-centered policies for personal health records.

Telehealth specialist Coviu has partnered with health monitoring software vendor The Clinician to launch an integrated telehealth and remote patient monitoring solution for general practices for the management of COVID-19 patients in the home.
The solution is similar to a hospital-in-the-home care model and will allow GPs and practice nurses to remotely monitor patients and their symptoms with Bluetooth devices and symptom recording, as well as consult with patients directly through a video call if necessary.

International patient summary, NHS Digital and NHSX axed, Ireland’s plans for health data sharing, Singapore’s COVID certificate, EMR notes and overtime, Vocera and Amazon team up for Alexa in hospital, medical device bias
One step closer to interoperability: applying SNOMED CT’s engine to the international patient summary
Korea Bizwire ~ Staff writer ~ 25/11/2021
At SNOMED International’s recent October Business Meetings held in London, the organization’s governance bodies enacted a decision to extend the core of SNOMED CT’s structured clinical terminology to deliver an open, standalone sub-ontology to support the scope of content within the International Patient Summary (IPS.)
Long-awaited Wade-Gery review into NHS IT organisations is published
Digital Health News ~ Jon Hoeksma ~ 24/11/2021
The review states that despite much good work, digital transformation is currently fragmented across the system, split between different agencies and is “often overshadowed by requirements of the day-to-day”.

Victoria has moved along at a rapid pace in releasing a tender this week for its planned health information exchange (HIE), the first step towards streamlining access to medical records across the public hospital system. As locals like to argue incessantly, Victoria’s devolved public health system has positives and negatives, but the COVID-19 pandemic has certainly shown up that disparate information systems and services can be a drag on a unified pandemic response.
As such, earlier this year the Crisis Council of Cabinet agreed to a plan to consolidate pathology services across Victoria, including the different laboratory information systems (LIS) that are used in the state, of which we are aware of at least four, all in various instances that do not speak to others. NSW is in a similar situation, and it is looking to consolidate its LIS systems through the NSW Single Digital Patient Record (SDPR), the successful vendor for which is due to be announced shortly.

New Zealanders will be able to request assistance in getting a My Vaccine Pass from community pharmacies as the Ministry of Health opens up additional options for people to obtain one.
They can also request a pass be posted to them or emailed by calling 0800 222 478, with extra capacity added to call centres to help with demand.

Hospital billing and costing systems specialist PowerHealth Solutions has received its notice of integration (NOI) for claiming through Medicare’s new web services.
PowerHealth’s enterprise-level patient billing system, PowerBilling and Revenue Collection (PBRC-IE), is now web-services functional for bulk billing to Medicare, Department of Veterans Affairs claiming, overseas claiming, patient verification and eligibility checks, inpatient medical claims to health funds, and in hospital claims for both public and private facilities.

SA Pathology has signed a $25 million, seven-year contract renewal with Cerner for its statewide Enterprise Pathology Laboratory Information System (EPLIS), which will see the statewide public pathology provider move to a cloud-hosted, managed services environment.
The renewed contract will include Cerner’s remote hosting option (RHO) including disaster recovery, application managed service (AMS) for systems enhancements and upgrade services to ensure the software remains current, as well as other enhancements.

The Australian Department of Health has reminded prescribers and dispensers for what it says is the final time that image-based prescribing will come to an end on December 31.
The temporary measure was introduced at the start of the COVID-19 pandemic to allow prescribers to send a photo or fax of a prescription to pharmacists without the need to post a paper copy.
The department has backtracked on the issue before but says it will definitely end in 2021. It has agreed to continue the SMS subsidy until June 30, 2022.
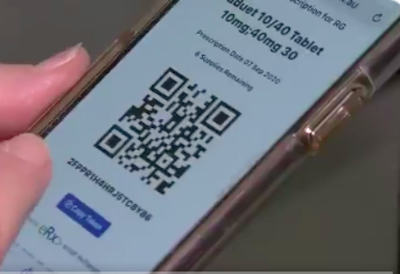
The use of electronic prescriptions has surged since June, when new lockdown provisions were introduced in NSW, Victoria and the ACT, and have now gone beyond 20 million eScripts issued since the new functionality went live in June 2020.
Prescription exchange service vendor eRx Script Exchange is reporting that 20 million eScripts have been issued since Australia launched national electronic prescriptions 15 months ago.

The West Australian Department of Health has gone live with its expanded statewide telestroke service, which is providing access to consultant neurologists by phone as well as real time access to an integrated communication and image viewing solution.
This solution allows doctors rural, remote and outer metropolitan areas to remotely transfer CT images, data, documentation and visual diagnosis of the patient to a dedicated statewide stroke consultant.

The Victorian Department of Health has gone to market for a commercial off the shelf Health Information Exchange (HIE) to allow the sharing of pathology data across the Victorian public healthcare system.
The HIE will support DH’s pathology reform program of work, which intends to consolidate existing public hospital pathology services into a small number of pathology service networks, as well as its laboratory information systems (LIS).
There is also the potential for the HIE to be used for sharing other clinical information, subject to the passage of the Health Legislation Amendment (Information Sharing) Bill 2021, which is currently before Parliament.
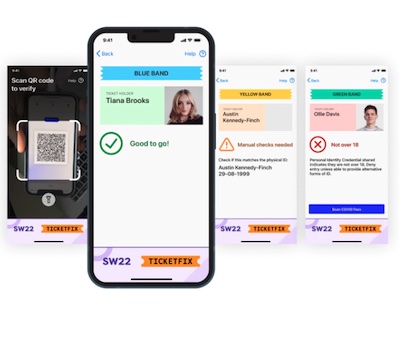
More than one million Kiwis have applied for the country’s My Vaccine Pass since the MyCovidRecord.health.nz site went live last week, with a trial of the technology to begin at hairdressing salons and barbers in Auckland from this Friday.
Prime Minister Jacinda Ardern announced today that New Zealand will move into its new traffic light system on December 3, taking over from the previous alert levels framework.

Practice management software vendor Medtech Global has received its notice of integration (NOI) from Services Australia for Medicare web services, which will be available in version 15 of Medtech Evolution at the end of the month.
Services Australia is moving its digital channels from a client adaptor-based system to online claiming over the internet using web services, with the client adapter shutting down in March 13, 2022.

Germany lags on digital health, equity and access in virtual care, Medtronic eyes digital health, Sweden launches vax pass, Vocera and Amazon team up for Alexa, interoperability in eight years, “dismal” cybersecurity in healthcare
Pandemic stress-tests Germany’s two-tier health system
Financial Times ~ Joe Miller ~ 18/11/2021
An OECD ranking of the health information available to policymakers in individual countries found that only Ireland was worse than Germany, among European countries.

Pulse+IT celebrated its 15th anniversary just a few months ago and while we don’t like to reflect too much on the damage those long years have wreaked upon our good looks, modest charms and superior intellect, it would be remiss of us not to mention some of the dashed promises and forlorn hopes that have accompanied our journey.
Our first issue was printed in August 2006, featuring a glamorous photo of a Canon camera and a rather unpleasant skin cancer to illustrate a story on digital clinical photography, along with the wise words of our first ever covergirl, then health minister the Hon Mr Tony Abbott.

Sydney’s St George Hospital has used the myBeepr clinical collaboration platform rolled out earlier this year to help it with role-based messaging and the hospital’s ward-based response to COVID-19.
At St George, patients suspected or diagnosed with COVID-19 flow through a streamlined process and are assigned to a COVID-19 care team and transferred to a dedicated COVID-19 ward directly from the emergency department.

South Australia is live with the first phase of its statewide secure messaging service, which is using HealthLink’s Fast Health Interoperability Resources (FHIR) standard-ready system to allow clinical documents to be sent and received via secure message delivery (SMD) irrespective of messaging vendor.
It is being used initially to send discharge summaries to GPs from hospitals either using the Sunrise EMR from Allscripts or the legacy OACIS electronic ordering and diagnostic results viewing system, which is predominantly used by Country Health SA’s regional hospitals.
South Australia went to tender for the solution in 2019, with HealthLink chosen as the successful vendor in 2020. The solution will roll it out to the whole state to handle the exchange of clinical documents such as discharge summaries and eReferrals between the state's hospitals and GPs.

New Zealand-headquartered healthcare technology investment firm Acclivis Group has bought Sydney-based community pharmacy software vendor Z Software in its first Australian investment.
Z Software’s dispensary, retail, back office and head office product suite is used by about 1000 community pharmacies across Australia.

Queensland-headquartered Direct CONTROL has built an online pre-admission questionnaire (PAQ) facility for hospitals and specialists using its Direct CONTROL Medical (DCM) application, as well as an online informed financial consent (IFC) for both hospitals and medical providers.
DCM includes both a provider and patient portal that gives users the choice of a Windows desktop experience or browser access from any device.

Rauland Australia will install its Rauland Responder Nurse Call and Master Clocks solutions at Acurio Health’s $100 million The George Centre private paediatric and maternity health facility being built in Sydney, which is due to open in 2023.
The George Centre will be one of the largest private hospitals in Sydney and the only private paediatric facility in NSW. Acurio also runs the Norwest and Sydney day hospitals.

Telstra’s health IT arm Telstra Health is aiming for revenues of $500 million by the 2025 financial year, and has also set its sights on further international expansion following its joint venture with PowerHealth Solutions.
In addition to revenue from its recent purchase of MedicalDirector, the company is seeing rapid growth in its virtual health and remote monitoring solutions, as well as in residential aged care, where it is the market leader.

The ACT government using its new Digital Health Record to help monitor COVID-19 patients at home.
COVID-positive patients who are isolating under the ACT COVID Care@Home program are able to monitor their symptoms and connect with their care team in real-time through the MyDHR app.

Digital claim payment platform LanternPay has partnered with medical billing API specialist Claiming.com.au to give healthcare providers access to the full suite of Medicare Web Services.
This includes Medicare bulk bill and patient claims (PCI), Department of Veteran Affairs (DVA), Eclipse and the Australian Immunisation Register (AIR) using either Claiming.com.au’s integration or the LanternPay portal.

ASX-listed online booking and directory service 1st Group has signed an agreement with St John of God Health Care to roll out its MyHealth1st EasyReferrals specialist solution, initially to two of its hospitals.
MyHealth1st EasyReferrals allows GPs and patients to search for a specialist based on the specific needs and area of specialisation and to see the specialist’s actual available appointments. The solution allows them to book the appointment and attach the referral documentation.

India starts digitising records, Philippines heads into health IT, riskiest devices in healthcare, digital technology in resource-poor nations, China regulates online healthcare, remote blood pressure monitoring in NHS, GE to spin out healthcare division, medical device incident response playbook
Centre starts work to digitise records
Hindustan Times ~ Rhythma Kaul ~ 11/11/2021
The Union health ministry has started the registration of all government medical facilities and doctors under the Ayushman Bharat - Digital Health Mission (ABDHM), a process that involves the digitisation of their information, including health records.
House OKs bill on telemedicine, eHealth on second reading
Philippine News Agency ~ Filane Mikee Cervantes ~ 10/11/2021
The House of Representatives on Wednesday approved on second reading a measure establishing the electronic health or eHealth system in the country using information and communications technology.

We must admit that we are still scratching our heads at Australian health minister Greg Hunt’s recent announcement of a new $180 million package to support COVID-19 care in the community in the future. There are some interesting bits, such as the subsidy for pulse oximeters for positive patients to use at home, and a small amount of money for medical deputising services and district nurses to visit COVID patients at home.
But putting aside the fact that there is simply no excess workforce capacity for nurses to visit people at home, let alone GPs – medical deputising services may be in a different boat – nor can we find a compelling reason behind the announcement that GPs will be paid an extra $25 to see COVID-positive or suspected COVID-positive patients face to face, in addition to existing MBS items.

All four district health boards in the Northern region are now on the same instance of the regional clinical portal, with Northland DHB recently going live with the upgrade.
Waitematā and Counties Manukau DHBs upgraded to Orion Health’s Clinical Portal 8 in 2018 and Auckland went live last year.

Medical indemnity insurance provider Avant Mutual has formally announced its partnership with healthcare communication platform myBeepr, which has been rolled out to 10 hospitals this year, including St George Hospital in Sydney and Western Health in Victoria.
Avant made a strategic investment in myBeepr a number of years ago and has since been working in partnership with the myBeepr team to evolve the product to improve clinical collaboration and communication.

The Australian Digital Health Agency (ADHA) has awarded a $2.1 million contract to Adelaide-headquartered IT consulting firm Chamonix to develop its digital health mobile channel, which will provide a mobile-native consumer app for the My Health Record system and other digital health initiatives.
Chamonix first developed the HIPS technology that enables the majority of state and territory hospitals to connect to My Health Record, as well as the first mobile app, Healthi, to link to the MyHR through myGov.

WA Health's ICT services agency Health Support Services (HSS) is looking for a new chief information officer after recently appointed CIO Christian Rasmussen resigned after less than a year.
Mr Rasmussen was appointed in January after his predecessor, Holger Kaufmann, also unexpectedly resigned after two years in the role.

Not only are patients expected to isolate at home, but GP practices are expected to look after patients in their homes.

NSW Health has kicked off the first phase of the statewide roll-out of its new SafeScript NSW real-time prescription monitoring system, with prescribers and pharmacists in the Hunter New England and Central Coast regions invited to register to use it.
Built by Fred IT and based on Victoria’s pioneering SafeScript system, SafeScript NSW will roll out to the other NSW regions over the next six months.
Unlike some of the other states, NSW does not plan to make the use of the system mandatory at this stage, although the collection of prescription and dispense data from the two prescription exchange services for the system is.

Medical specialist and day surgery software vendor Medical Wizard is now conformant with the Australian Digital Health Agency’s (ADHA) register of software able to provide electronic prescriptions by SMS or email.
Medical Wizard CEO Duminda Weerakoon said the feature allows doctors to prescribe medications to patients at the end of a telehealth consultation with just a few mouse clicks, and the patients will instantly receive the prescription.
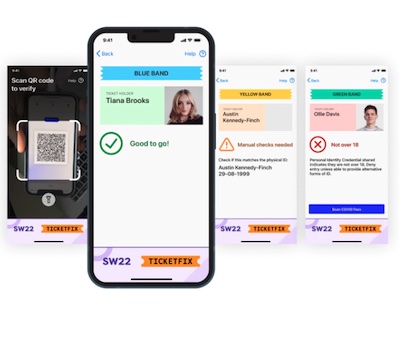
The New Zealand Ministry of Health (MoH) has released specifications on its GitHub account to help Kiwis understand the technology behind its My Vaccine Pass, the official record of a person’s COVID-19 vaccination status.
MoH plans to release a separate pass for international travel shortly, both of which will be stored in a QR code that can be downloaded to phones or printed out.

University of Sydney researchers and the Sydney Children’s Hospital Network (SCHN) have developed an internet of things-powered e-Gate solution that provides a screening and contract tracing process before people enter hospital.
The e-Gate smart sensing system is aimed at improving the safety and efficiency of health screening check-points at large organisations such as hospitals. Hospital visitors can use the system by registered at home before arrival, and it can also be used as a rapid staff screening solution.

A registered nurse working in a Perth COVID-19 respiratory clinic has been charged with fraudulent recording of vaccine information after allegedly faking a COVID-19 shot for a teenager.
The nurse is alleged to have obtained approval from her employer to administer COVID-19 shots to family and friends, including the teenager, and administering the injections behind closed doors.

Adelaide-based patient pathways software vendor Personify Care has partnered with Propell Health, distributors of iHealth devices in Australia, to integrate its system with wireless pulse oximeters to support virtual models of care for COVID-19 patients isolating at home.
Pulse oximeters are soon to be subsidised by the Australian government to allow GPs to monitor patients in the community, but they are also commonly used for remote monitoring and hospital in the home programs by hospitals and public health services.

Trust in EMR data, Philips’ Tasy vulnerability, France’s fourth COVID pass, Egypt’s COVID app, NHS Covid Pass accepted by EU, new CIO for US VA as Cerner EMR modernisation program under scrutiny, saving time with Microsoft Teams, English standard for medicine message content, lack of uniform standard for telehealth
80% of IT hospital execs don't fully trust their hospital's EHR data
Becker's Hospital Review ~ Hannah Mitchell ~ 28/10/2021
Hospital executives said they lack fully reliable and interoperable data despite their potential in driving decision-making, according to a Sage Growth Partners report.

The FHIR standard was back in the spotlight this week with the ongoing fall-out from the recent publication of a super duper report into vulnerabilities that may eventuate from poor implementations of the standard by third parties.
Last week, HL7 International took what is a very unusual step in releasing a statement emphasising that the vulnerabilities are at the implementation end and certainly not at the standard itself, and touting that the author had changed the title of her report to reflect this.

A year after its go-live with its TrakCare electronic medical record from InterSystems, Bendigo Health is reaping the benefits of the ability to implement a new way of managing clinical data and integrate it across the hospital with a range of other clinical information systems.
The new $650 million Bendigo Hospital went live with the EMR last November, having delayed the planned implementation in March 2020 due to the coronavirus pandemic.

Six hospitals in the Loddon Mallee region of Victoria have gone live with the Charm Evolution shared electronic oncology solution from Citadel Health.
Loddon Mallee signed a five-year agreement with Citadel to streamline more than 10,000 chemotherapy treatments episodes each year using Charm Evolution, including Mildura, Bendigo, Echuca, Swan Hill, Kerang and Kyneton hospitals.

The Australian Digital Health Agency (ADHA) is holding an industry briefing on November 4 to explain its latest offer to the software industry to assist it in better integrating with My Health Record, including adding an aged care transfer summary to the system.
Plans are also underway to develop industry standards for software used in aged care and general practice, as well as electronic medication management systems, and to support the use of secure messaging in the aged care sector.

Medical specialist software vendor Genie Solutions has updated its integration with the My Health Record system to improve the user experience for specialists, enabling doctors to launch MyHR directly via the Australian Digital Health Agency’s HIPS viewer from within Genie and the cloud-based Gentu system without the need to download documents.
Genie Solutions has had an integration with My Health Record in its Genie clinical information system since 2012, but uptake of the MyHR – then known as the PCERH – has been low from the specialist sector.

Royal Adelaide Hospital and The Queen Elizabeth Hospital have implemented eight digital patient pathways co-designed with local firm Personify Care to relieve pressure on frontline staff by digitising previously manual clinical protocols.
Personify Care worked with the Central Adelaide Local Health Network (CALHN) on the roll-out for CALHN patients in more than 20 speciality areas across the two hospitals, as well as SA Dental.

InterSystems has released an innovation toolkit for its TrakCare healthcare information system to give users easier access to patient data using the IRIS for Health FHIR repository.
The aim is to will allow users to quickly start working with SMART on FHIR apps and unlock data held in TrakCare.

The Australian government has released a new package of funding to provide assistance to GPs and practice nurses, along with subsidies for devices like pulse oximeters, as the management of COVID-19 cases moves from hospital to the community.
Health Minister Greg Hunt said the package would also include extra support for Healthdirect to support COVID-positive treatment pathways in community care.

Eight appointment booking solutions have signed contracts with Healthdirect to implement an application programming interface (API) to connect vaccination clinics with real-time appointment availability through Healthdirect’s Vaccine Clinic Finder.
Separately, the Australian Department of Health is running a trial of a new Vaccine Clinic Finder Connect capability, which is using PRODA account security to enable clinic details to be self-managed and updated directly to the Vaccine Clinic Finder.

NHS app takes off, appointment booking system hacked, tech not enough for long-term care, US grapples with telehealth payment regulations, Amazon’s Alexa in health and aged care, £2bn for digital NHS, REvil ransomware taken down
Almost 28 million people in England are now registered with NHS login
Digital Health News ~ Cora Lydon ~ 25/10/2021
The online service is managed by NHS Digital and gives registered users a secure single point of access to 45 apps and e-health services.

Pulse+IT was a keen attendee at this week’s Health Information Management Association of Australia’s (HIMAA) annual conference, which naturally in this pandemic era was held virtually. It was pretty good too, and revealed quite a lot of information about Victoria’s digital health roadmap, which was launched back in August but got little if any coverage due to the pandemic itself.
The roadmap is in no way a grand, sweeping vision like others purport to be but is instead built around existing projects – most of which have been precipitated by Stephen Duckett’s Targeting Zero review of hospital safety and quality assurance from 2016 and the more recent Royal Commission into Victoria’s Mental Health System – and turns out to be a pragmatic, practical strategy that takes into account the decentralised nature of the state’s health service.

New Zealand Auditor-General John Ryan has formally rejected an application by Orion Health CEO Ian McCrae to audit the Ministry of Health’s procurement of the COVID immunisation register (CIR) and the national immunisation solution, as well as the national screening solution (NSS).
Mr McCrae requested an audit in May, saying the ministry had ignored normal procurement processes and had used incorrect information in its business case. He also criticised the $38 million price tag for the overall infrastructure.

Health IT standards-setting body HL7 International has taken the unusual step of issuing a clarifying statement about the release earlier this month of a report by a cybersecurity expert into vulnerabilities she exposed in third-party implementations of application programming interfaces (API) using the Fast Healthcare Interoperability Resources (FHIR) standard.
Las Vegas-based expert Alissa Knight of Knight Ink published a report this month called “Playing with FHIR: Hacking and Securing FHIR APIs", which detailed a year-long exploration of vulnerabilities in a number of implementation of apps using FHIR APIs.

It may have flown a bit under the radar during the COVID-19 pandemic, but Victoria has made a good start on its five-year digital health roadmap, which aims to improve the safety and efficiency of Victoria’s healthcare system.
The roadmap, released in August, includes five programs of work, of which three are well underway. These programs include existing initiatives such as the roll-out of a statewide unique patient identifier, as well as the plan for statewide sharing of clinical information, with a bill currently before the upper house to allow an amendment to the Health Services Act 1988.

Queensland’s real-time prescription monitoring system QScript went live last month and is mandatory for GPs and pharmacists to check when prescribing or dispensing drugs of addiction from tomorrow.
QScript is the third roll-out of the system first developed for RTPM in Victoria, where it is known as SafeScript. South Australia has also implemented a similar system, dubbed ScriptCheckSA.

The Australian Digital Health Agency (ADHA) is planning to add an aged care transfer summary (ACTS) to the My Health Record system to enable digital capture of a residential aged care facility (RACF) patient’s health information when transferring from aged care to another health facility or back to their home.
It also plans to develop an aged care clinical information system standard, and to support the clinical systems used in aged care and general practice, as well as electronic medication management systems, to enhance their solutions to include MyHR integrations.

The Victorian Department of Health (DH) is re-establishing a digital health design authority to help manage its digital health roadmap, one of the key focuses of which is the roll out of a health information exchange (HIE) to securely store and present clinical information to support patient care across the public healthcare system.
DH has already established a laboratory information system design authority called LISConnect to support an HIE for sharing pathology results across the state. This will see the multiple Victorian Public Health Services (VPHS) pathology services consolidated into three new Victorian Public Pathology Services (VPPS), with funding provided through the LISConnect program for the implementation of an integrated LIS and HIE.

Practice management system vendor MediRecords has partnered with telehealth device and technology firm Visionflex to integrate the Vision video conferencing platform into MediRecords’ cloud-based solution.
The integration will enable health professionals to perform clinical telehealth examinations and automatically save patient data to their patient records, the vendors say.
Eastern Health is extending its emergency department capability through a new model of care using My Emergency Doctor’s virtual emergency specialists, rolling out the service for low-acuity patients at Box Hill Hospital and shortly to Maroondah and Angliss hospitals.
Eastern Health nurses will triage patients presenting at the ED and direct stable and non-urgent cases to a remote specialist, who then assesses them in a private room using a web-enabled device. Specialists can write prescriptions for the patient if necessary.

New York’s Excelsior vaccine passport, FHIR APIs vulnerable to hacking, France’s digital health space, US national patient ID, diabetes data in smartwatches, Scotland makes digital solutions free, Israel urges hospitals to print out medical files, mHealth for blood pressure
How New York overengineered its million-dollar vaccine passport
Recode ~ Rebecca Heilweil ~ 21/10/2021
Not many businesses are using the Excelsior Pass’s signature feature: a scannable QR code that can quickly verify customers’ vaccination status by checking state records.
Security flaws in health apps, APIs potentially put millions of patient records at risk, report finds
FierceHealthcare ~ Rebecca Torrance ~ 20/10/2021
Third-party apps and aggregators that pull data from electronic health record systems may be vulnerable to hacks, putting millions of patient and clinician records at risk, a new report found.

Hāwera Hospital is set to go live with a pilot of the Better Meds medications management platform next month, which if successful will roll out to all five Te Manawa Taki (TMT) district health boards.
The solution is replacing the MedChart solution from Dedalus currently used by Taranaki DHB.

In the real world, Australia and New Zealand began to put into action their respective roadmaps out of lockdown this week as vaccination numbers rose to much hoped-for levels. However, in the somewhat obscure world of health IT standards, a quite remarkable report was released late last week that has stimulated a firestorm of debate over the basic security of healthcare data.
Las Vegas-based cybersecurity analyst, former hacker and content creator Alissa Knight – who going by her bio and her Knight Ink business description is surely to become the subject of a novel one day if not a pretty cool movie – released the second phase of a year-long research project she has undertaken into the basic security of apps and aggregators drawing data from FHIR APIs linked to electronic medical records and other patient record databases.

The Accident Compensation Corporation (ACC) will migrate its operations across to Microsoft’s Azure cloud service, following an all of government agreement between the New Zealand Department of Internal Affairs and Microsoft earlier this year.
The three-year cloud services agreement will see ACC migrate its New Zealand operations to Azure.

The Office of the Australian Information Commissioner received just seven privacy complaints relating to the My Health Record in 2020-21 and only three data breach notifications – two of which were resolved – in the same period.

Community pharmacy banner group Sigma Healthcare will roll out HealthEngine’s Patient Appointment Management System (PAMS) to support online bookings, scheduling and voucher management at its Amcal and Guardian outlets.

The Australasian Institute of Digital Health (AIDH) is surveying healthcare organisations to check on improvements to cybersecurity since its last survey four years ago, as the Australian government moves to impose a stronger reporting regime to battle ransomware.

Online booking platform HealthEngine is getting ready to list on the stock exchange, while competitor HotDoc is also looking to raise new capital, both boosted by turnover due to the massive increase in vaccination bookings during the COVID pandemic.

St Vincent's Hospital emergency doctor and former AMA vice president Stephen Parnis is headlining the Health Information Management Association of Australia (HIMAA) annual conference next week, discussing why health information matters in a time of pandemic.
Dr Parnis will be joined by Victoria’s chief digital health officer, Neville Board, and Australian Digital Health Agency CEO Amanda Cattermole.
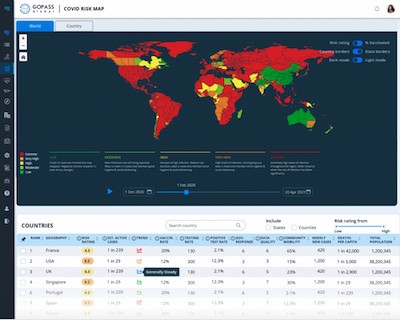

Microsoft is building an artificial intelligence-powered data analytics platform in association with biosecurity risk analytics vendor GOPASS Global to provide intelligence on the risks in international travel to COVID-19 hotspots as Australia and New Zealand release plans on opening borders to international travel.
The GOPASS Global pre-travel risk management platform uses a Microsoft data lake to take in information from 35 different sources, covering 240 countries 3900 airports and more than 700 airlines.

The Australian government will go live with a new system from tomorrow to allow Australians and Australian visa holders who have a valid passport and their COVID-19 vaccination recorded on the Australian Immunisation Register (AIR) to obtain an international COVID-19 proof of vaccination.
The pass will enable fully vaccinated Australians to depart Australia and to travel internationally, and is compatible with COVID-19 travel apps such as the International Air Transport Association (IATA) travel pass.

Sydney Local Health District has expanded its contract with Alcidion to use its Miya Precision remote patient monitoring platform to monitor patients with acute diverticulitis in addition to those with COVID-19, and will also deploy a patient app to better engage with patients.
Sydney LHD first signed an agreement with Alcidion to use Miya Precision to support COVID-19+ patients at home through virtual care, managed by the RPA Virtual Hospital (rpavirtual), at the height of the first wave of the pandemic.

Digital health in China, Italy’s COVID health pass mandate, AI for TB in Africa, OCHRE for mobile apps, tech and GP burnout, tech and practice staff burnout, Cerner on EMR usability, open source collective for digital health, FIN12 ransomware targeting healthcare
China’s data-driven dream to overhaul health care
Nature ~ Sarah O’Meara ~ 06/10/2021
Collaborations between AI researchers and China’s medical workers are helping to combat diseases such as diabetes and COVID-19.
‘COVID health pass’ required for Italian workers starting next week
Voice of America ~ Jamie Dettmer ~ 08/10/2021
Starting next week, all public and private workers in Italy will be required to have a digital COVID-19 health certificate or face being sent home on unpaid leave and fined up to $1,730.

A landmark report in Australian healthcare was handed down this week with the release of the recommendations from the independent Primary Health Reform Steering Group on the federal government’s primary healthcare plan for the next 10 years.
The report is very much influenced by the Department of Health’s voluntary patient registration (VPR) model, which seems to have taken over as preferred policy from ideas like Health Care Homes and patient-centred medical homes. (It’s interesting that GPs who have in the past railed against the idea of capitation seem to be quite keen on VPR, but that’s a discussion for another day.)

New Zealand’s Ministry of Health has officially gone live with its new My Covid Record website, which will allow people to view their records and eventually download proof as a vaccination pass.
MoH’s group manager for national digital services Michael Dreyer said the exact timing for when and where vaccination proof will be required is still being finalised but the site was now live.

The Australian Department of Health has released a draft of its 10-year plan to reform primary healthcare, which in a surprise move ties MBS-funded telehealth to its delayed voluntary patient registration (VPR) system.
VPR is supported by the Royal Australian College of General Practitioners (RACGP) but its introduction has been delayed due to the coronavirus pandemic. It would see patients with chronic conditions voluntarily registering with one general practice, which would receive service incentive payments paid to improve the patient’s health rather than the current fee for service system.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.