
It came as a bit of a surprise this week to see that Hills Ltd, formerly of hoist fame and for some time now a player in nurse call, patient infotainment and security IT solutions, had taken a majority share in Extensia, the small Brisbane firm that developed the RecordPoint shared care record. We haven’t heard from Extensia in years and thought they’d gone out of business, but up they popped in an industry survey on Tuesday as a case study for medical software’s value during the COVID pandemic in Australia.
Hills actually took the stake back in November 2021 but is only promoting it publicly now, new Hills CEO David Clarke tells us. The move is part of a renewed focus on the health sector for Hills, which is planning to divest itself of the security IT business, its most profitable asset. Hills has some quality contracts for its patient infotainment, hospital TV and nurse call systems in both hospitals and aged care, as well as a distribution agreement with US firm GetWell for its patient engagement products, but clinical software is a new venture for the company. The company has also cleared two long-standing, multi-million dollar legal actions against it, one dismissed by the Federal Court and the other resolved to everyone’s mutual relief.

ASX-listed Hills Ltd has quietly bought a majority share in Brisbane-based Extensia, heralding a renewed focus on its healthcare assets as it divests its security IT division.
Extensia, which makes the RecordPoint shared care software system, has been in the market for close to 20 years but has been dormant for some time. Hills took a 70 per cent share in the company in early November 2021 but is only now publicly promoting the purchase.

Lyniate, the newly named US owner of the Rhapsody integration engine first developed by Auckland firm Orion Health, has entered into a merger agreement with NextGate, which markets identity resolution and enterprise master person index systems widely used in Australia and New Zealand.
Orion Health was forced to sell its crown jewel in Rhapsody in 2018 when it delisted from the Australian stock exchange. Rhapsody was sold to British private investment firm Hg that year, and in 2019 was merged with American healthcare integration company Corepoint Health, later renamed as Lyniate.
Adelaide-based day hospital software vendor Clintel Systems has made a number of upgrades to its CareRight Day Hospital suite, including transitioning all users to the new Medicare web services system and introducing a new patient interactive module (PIM) for patient pre-admissions.
Clintel also plans to release electronic prescribing functionality in the next couple of months.

ASX-listed medication management app and pharmacy services software vendor MedAdvisor has entered the New Zealand market, signing a deal with NZSX-listed pharmacy and medical services provider Green Cross Health.
The three-year deal involves making MedAdvisor’s technology available to 350 community pharmacies under Green Cross Health’s Unichem and Life brands, comprising about 40 per cent of the NZ market.

Gold Coast Primary Health Network (GCPHN) has announced it will prioritise the installation of its Primary Sense data extraction tool at general practices in its region using compliant software, and will no longer fund licences for rival products from commercial vendor PenCS.
GCPHN has been developing Primary Sense for the last five years as a population health management and clinical audit tool, and is currently being used by 83 practices.

General practices in three primary health network areas are being invited to take part in a trial of a digital clinical decision-support system that uses data from general practice records to prompt risk-based screening of people living with chronic viral hepatitis.
The HepLOGIC trial is funded by the Victorian Cancer Agency and involves the Royal Melbourne Hospital, the Doherty Institute, and the Gippsland, Eastern Melbourne and South Eastern Melbourne PHNs, using technology and data analysis from Outcome Health through its POLAR tool.

The Medical Software Industry Association (MSIA) is calling for fairer procurement processes and more funding for health technology companies, saying its members believe the federal government stifles innovation and that Australian companies are disadvantaged compared to multinationals.
In a pre-budget and pre-election statement, the peak body claims the sector still remains “unsung and invisible” despite its role in developing and implementing technologies for the COVID-19 response.

The Aged Care Industry Information Technology Council (ACIITC) has put out a call for aged and community care providers to take part in three new national roundtables, aimed at increasing the uptake of technology and innovation in the industry.
The national roundtable focus areas are technology specific considerations; service model and workforce reform; and financial considerations, including return on investment research and development.

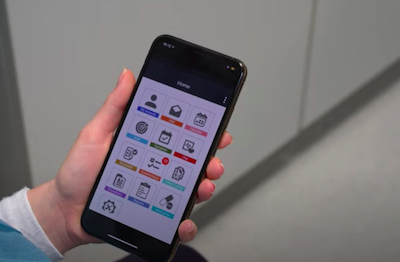
WA Health will make its Manage My Care outpatients appointments and referrals app available to the whole state over the next few months following a successful pilot in 2020 and a roll-out to all metropolitan hospitals over the last two years.
The app, developed by NEXA Group, is integrated with WA Health’s statewide patient administration system, Dedalus's WebPAS. Every WA public patient has a unique patient identifier and information associated with their healthcare history is available through linked clinical applications.

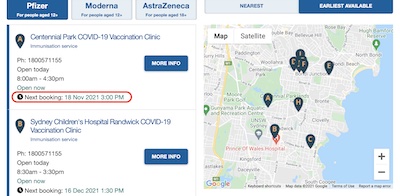
Practice efficiency and appointment booking system vendor AutoMed Systems has integrated its booking system with Healthdirect Australia’s Service finder, allowing real-time appointments beyond COVID-19 vaccinations to be displayed and booked directly.
The service has been rolled out to the urgent care clinics in Western Australia using AutoMed and is now being provided to all of AutoMed’s wider customer base free of charge.

Epic CEO on interoperability, EMR market share in the US, digital health reform in the UK, NLP in Google’s Care Studio Conditions, remote patient monitoring in the mainstream, controlled drugs and telehealth, social robots in paediatric hospitals, Germany's Digital Health Care Act
Epic CEO: We are now interoperable with the world
MedCity News ~ Arundhati Parmar ~ 10/03/2022
Epic CEO Judith Faulkner aimed to set the record straight about Epic's capabilities in AI, interoperability as well as describe what developments she is excited about in healthcare.

The NZ Ministry of Health has responded to criticisms from GPs about the functionality in its Covid Clinical Care Module (CCCM), which is being rolled out to help healthcare providers to care for COVID-positive patients in the community.
The CCCM has been adapted for use from the Border Clinical Management System (BCMS) developed by Valentia Technologies using its indici PMS, and is designed to create visibility of the care provided so that people with COVID-19 can access care when they need it. It is also being used in some areas to support payment mechanisms.

The devastation inflicted on northern NSW and Queensland during the floods over the last fortnight has been heartbreaking to watch. Having spent some time in Kyogle and the northern rivers of NSW as well as southern Queensland, Pulse+IT is finding it hard to imagine the horror that the people and animals of the region have gone through.
While tertiary health services seem to have survived quite well, the same can’t be said for the fate of many primary healthcare providers, who are after all the lifeblood of regional communities. General practices, pharmacies, community and Aboriginal health centres and allied health have had their premises and their businesses swamped and destroyed. The pictures of elderly people from residential aged care facilities still dressed in their pyjamas being rescued in dinghies and carried to safety by locals and Pacific Island seasonal workers is reassuring. The images of the total destruction of the town of Lismore is not.

Tasmania will continue to use the TasVax system from Oracle for other public health-delivered vaccination programs such as the annual flu vaccine and school-based vaccination programs following the well-accepted COVID-19 vaccination system it enabled in just six weeks in early 2021.
The Tasmanian government contracted Oracle on a public good basis – offered by Oracle – to develop a state-wide solution to vaccinations in late 2020, having surveyed the major players. With limited funds, the state decided on a fast procurement process that ruled out a lot of the smaller vendors, but also limited its options in terms of large companies.

The Digital Health Cooperative Research Centre (DHCRC) has lost its third chief executive officer in four years, with Adelaide-based Terry Sweeney resigning suddenly this week.
The CRC has appointed Research Australia chair and former Bupa Health Foundation executive lead Annette Schmiede (pictured left) as acting CEO.

The Australian government will decommission the much-vaunted national booking platform for COVID-19 vaccinations at the end of May, along with the Commonwealth Vaccine Integrated Platform (CVIP) developed by the Australian Digital Health Agency for clinics without access to the Australian Immunisation Register (AIR).
DoH awarded a $3 million contract to HealthEngine in March 2021 to provide a national booking solution for general practices and pharmacies that did not already use an online booking solution.

Clinical and practice management software vendor Best Practice Software has released the Medicare web services-enabled version of its Saffron release, which provides direct access to the Australian Immunisation Register from the patient record as well as online claiming functionality through Medicare web services.
Best Practice users were given an extension to the transition to the new regime through Saffron SP3 beyond the deadline of March 13, although they were required to sign up to PRODA and have new PKI certificates installed prior to that deadline.

NSW Health has launched a virtual care strategy that outlines its pathway for a coordinated and consistent approach to scale virtual care and integrating it as an option across the state.
While emphasising that virtual care is not new and is a complement to existing services, the strategy acknowledges that particularly during the COVID-19 outbreak in 2020, a rapid response was critical.

Melbourne’s Global Health has launched a new app called MasterCare Connect that provides clinicians with access to a lightweight version of its MasterCare electronic medical record when they are on the road or in a remote setting.
The app is designed to improve access to patient information at the point of care and provides clinicians with the ability to work both online and offline.

The Royal Victorian Eye and Ear Hospital in Melbourne has become the first hospital in Australia to implement the My Health Record system’s pharmacist shared medicines list (PSML).
The PSML is a consolidated list that includes information about prescription and non-prescription medicines such as over-the-counter and complementary medicines, including vitamins and herbal remedies.

Diagnostic imaging provider Synergy Radiology has in integrated Foxo’s secure healthcare communication and clinical workflow platform into its Kestral radiology information system (RIS) and rolled it out across its 10 imaging centres in Sydney.
Synergy Radiology deployed Foxo to improve clinical reporting efficiencies, reduce the administrative burden on its radiologists, and unify its clinical and clerical workforce.

Dedalus to drop Lorenzo in UK and Ireland, Harris Computer’s Allscripts purchase, Singapore’s health supercomputer, information blocking in the US, long COVID on social media, telehealth use during pandemic, telehealth revenue, AI in DI, online paediatric care, digital health in sub-Saharan Africa, EHRs in Ireland
Dedalus to replace Lorenzo EPR with Orbis software
Digital Health News ~ Jon Hoeksma ~ 03/03/2022
Health IT giant Dedalus has announced that it will cease offering the Lorenzo electronic patient record (EPR) system in the UK and Ireland and will switch to Orbis.
Allscripts to sell hospital and large physician practice assets
Healthcare IT News ~ Kat Jercich ~ 03/03/2022
Constellation Software's N. Harris Computer Corporation could pay up to $700 million for the business segment, which includes the Sunrise, Paragon, TouchWorks, Opal and dbMotion tools.

The big news in health IT this week was the proposed sale of EMR vendor Allscripts’ hospital assets to Harris Computer, a subsidiary of Canadian software company Constellation Software. Harris has been buying up a few interesting companies recently, including Sydney-based obstetric and maternity software developer Meridian Health Informatics.
Meridian’s software is used by NSW Health, Queensland Health and Tasmania’s Department of Health, and Harris also added in the UK’s K2 Medical Systems to the mix last year, with a view perhaps to hoovering up the hospital-based maternity market. But Allscripts is a much bigger kettle of fish, with EMRs implemented around the world and a healthy enough listing on the NASDAQ index.

Canadian software solutions firm Harris Computer has purchased the hospital and large physician practice assets of NASDAQ-listed electronic medical record vendor Allscripts for $US700 million ($A950m), including its Sunrise EMR suite and the Australian-developed Opal digital medical record, formerly known as BOSSnet.
Sunrise is used as the EMR and patient administration system for the largest hospitals in South Australia, while BOSSnet is used in a number of hospitals in Western Australia – including Fiona Stanley – and Victoria.
Medical specialist practice management software vendor Shexie says its Shexie Platinum system has received certification for access to the new Medicare web services connection method for online claiming, which is coming into force on March 13.
Shexie says the new functionality continues the connection between Shexie Platinum and Services Australia, allowing for integrated online claiming directly from within the software and without the need for any external applications or plug-ins in order to both send and receive information for online claiming purposes.

Aged care patient monitoring platform provider Health Teams has signed an agreement with respiratory disease app vendor ResApp Health to use its ResAppDx on Health Teams’ new telehealth platform and for in-room patient consultations.
Health Teams expects to launch ResAppDx on its platform in the second quarter of the year. The company says it is the only dedicated digital health platform in Australia for the aged care sector.

Tū Ora Compass Health and Pinnacle Midlands primary health organisations (PHOs) have set up a new telehealth after-hours service for network GP practices and patients, covering Wellington, Lower Hutt, Palmerston North and New Plymouth.
Practice Plus was launched last month co-designed with practice teams, and offers additional virtual access options to after-hours GP care on weekday evenings from 5-10pm and weekends 8am-8pm.
New Zealand’s leading primary care patient portal vendor has added a new function to its ManageMyHealth system, allowing patients and GPs to keep track of COVID-19 symptoms when being cared for at home.
My Health Diary lets patients go online and fill out information boxes about their symptoms, which can then be monitored by their GP, if necessary.

Adelaide’s The Queen Elizabeth Hospital (TQEH) has rolled out the Personify Care digital patient pathways platform across all of its elective surgery specialties following a successful trial in its endoscopy unit.
The hospital says it has been able to reduce patient waitlist times by 71 per cent using the digital patient pathways, which simplifies the waitlist, nursing and admin workload by digitising the pathway.

St Andrew’s Toowoomba Hospital has rolled out the Charm oncology information management system, said to be the hospital’s first centralised patient record combining reporting, appointment scheduling and treatment plans for about 50 oncology patients each day.
The 155-bed private hospital signed a three-year deal for Charm Evolution in 2021 on the recommendation of medical oncology and haematology practitioners.

Propell Health has added Biofourmis patient monitoring systems to its distribution network to provide hospitals with remote monitoring solutions for Hospital in the Home (HitH) programs.
Propell is the Australian and New Zealand distributor of iHealth devices and recently signed deals to integrate its technology with telehealth platform Coviu and patient pathway vendor Personify Care.

The ACT’s real time prescription monitoring system Canberra Script is now live, replacing the DORA system that has operated in the territory since 2019.
Two other jurisdictions – Tasmania and the Northern Territory – are also set to roll out similar technology for monitoring controlled drugs this year, with NTScript due to go live next month and TasScript later in the year.

Patient administration and billing solution vendor Direct CONTROL has achieved its notice of integration with Medicare web services for its Direct CONTROL Medical (DCM) application, developing a checklist so users can move from Medicare’s old client adaptor technology to the new web services system as easily as possible.
Healthcare providers need to move over to web services to access Medicare Online, including bulk billing, Department of Veterans Affairs claiming, overseas claiming, patient verification and eligibility checks, inpatient medical claims to health funds, and in hospital claims for both public and private facilities through ECLIPSE.

International vaccine certificate recognition, US vaccine pass, digital health plan for NHS England, online portal to return elective surgery to normal, EPRs for NHS Trusts, NIST guide to telehealth and RPM, racial bias in medical records, “transformative year” for health IT, says Micky Tripathi
WHO making moves on international vaccine 'passport'
Politico ~ Daniel Payne ~ 24/02/2022
The World Health Organization will convene member states and leaders of Covid-19 immunization credential technology groups to recognize different vaccine certificates across nations and regions.
Pulse+IT was out in force this week at the Digital Health Institute Summit in Melbourne, which for some of us was the first opportunity to see interstate human beings in person for at least the last two years. Unsurprisingly there was a pretty big turn-out, with double the numbers expected turning up amid familiar sights like long lines at the espresso coffee stands and non-existent lines for ye olde brewde coffee stande, understandable considering it offers warmed up sump oil and dishwashing water and not much else.
Despite a shortened agenda, the Australasian Institute of Digital Health’s program team managed to shoehorn in a great deal of pretty great content into the two days. Very little was dull (barring a speech by a regulatory agency representative, but that was to be expected), and we all learned a lot. It was all filmed as well so AIDH members can see everything online. There’s also a virtual showcase happening next week that will be streamed live.

It took a while to get there, but Victoria managed to roll out its integrated COVID-19 Vaccination Management System (CVMS) in a matter of months in 2021 as the first two vaccines were approved by the TGA and health services scrambled to conform with requirements to report every vaccine administered to the Australian Immunisation Register.
Rolling out the Microsoft technology across health services that used disparate electronic medical records – some still on paper – and having to implement booking systems never before used was a journey for many, not the least of which was Monash Health’s South Eastern Public Health Unit (SEPHU), which piloted the technology.
Consumer access to their own healthcare information is one of the five programs of work that the Victorian Department of Health has committed to under its digital health roadmap, and fortunately it has the experience of Melbourne’s Royal Children’s Hospital to call on, having rolled out a patient portal back in 2016.
The rest of the Parkville precinct hospitals are also using Epic’s technology for their portals, underpinned by a shared database across the precinct, and now Alfred Health is rolling out its own, using Cerner’s patient portal technology to link into the hospital’s EMR.

National public health information service Healthdirect Australia was naturally called into action as the coronavirus first started to emerge in early 2020, providing telephone advice to the worried public through its well established healthdirect helpline.
What was a little different about setting up what has since become known as the National Coronavirus Helpline (NCH) was the timeframe: just two weeks from start to go-live. And since it went live in March 2020, it has handled more than four million calls.

Healthdirect Australia has integrated its video call service with its existing GP after hours helpline to provide an additional service for patients seeking help during the pandemic, with numbers increasing from about 70 video consultations per week to over 300 since its inception.
Healthdirect Australia has run the nurse-led triage helpline healthdirect for a number of years as well as other services such as the My Aged Care call centre and the pregnancy, birth and baby helpline, and in the time of COVID, the national booking solution, symptom checker and vaccine clinic finder sites. It also set up the National Coronavirus Helpline in just two weeks in January 2020.

Researchers from the Centre for Health Analytics at Melbourne’s Murdoch Children's Research Institute are studying whether social media platforms such as Twitter can be used as a vaccine safety data source to pick up potential adverse events, not just for the COVID vaccines but potentially many paediatric and adult vaccines.
The research is looking at whether social media data can be added to existing data sources for the Surveillance of Adverse Events Following Vaccination In the Community (SAEFVIC) vaccine safety surveillance service.

Sydney Local Health District has launched a virtual wound care command centre to provide remote care for patients with chronic wounds who are receiving care supported by Tissue Analytics’ artificial intelligence-powered app.
Sydney LHD has been trialling the app at Royal Prince Alfred Hospital and Sydney District Nursing for several years and has integrated it into the hospital's Cerner electronic medical record so images and data can be stored, reviewed and compared.

Western NSW Local Health District is offering its new virtual clinical pharmacy service to all hospitals in the region following a successful trial that saw pharmacists provide consultations with patients via video conferencing and communications between clinicians using the electronic medical record and electronic medications management systems.
Western NSW LHD lead virtual pharmacist Brett Chambers told the Digital Health Institute Summit 2022 in Melbourne today that the model of care in the trial, which began just before the COVID-19 pandemic began, was designed around the high availability of teleconferencing at all health facilities in the district.

Victoria plans to kick off its digital health roadmap in earnest this year, with hopes that legislation underpinning its planned electronic health information exchange expected to pass the upper house in the next month or so.
Representatives from the Victorian Department of Health’s digital health branch told the Digital Health Institute Summit 2022 in Melbourne today that the roadmap covers five programs of work, including improving health services’ resilience against outages and cyber attacks.

Athenahealth sold for $17b, does India need an electronic health record? AI in the NHS, weeding out racial bias in AI, virtual care still popular with patients despite decline in use, budget to launch India’s Ayushman Bharat Digital Mission
EHR vendor athenahealth acquired by Hellman & Friedman, Bain Capital
EHR Intelligence ~ Sarai Rodriguez ~ 17/02/2022
Two private equity firms have acquired cloud-based EHR vendor athenahealth in a $17 billion transaction.

All the talk this week has been about the changing of the guard at Australia’s largest health IT company, with news that NSW Health secretary Elizabeth Koff will take over from her predecessor, Mary Foley, as the next MD at Telstra Health. Professor Foley was very warmly regarded by both her peers and her staff and in addition to setting the company on the path to profitability and buying up some pretty valuable assets, she has weathered a number of political storms with aplomb.
Telstra Health recently won a large contract outside of the healthcare industry – a $200 million, five-year deal to run Australia’s 1800RESPECT national assault, domestic and family violence hotline – signalling that it is now able to leverage some of the infrastructure it put into place for huge projects like the National Cancer Screening Register. It will be interesting in the next year or so to see how it handles the MedicalDirector transition (we are still convinced it paid too much) and its plans for international expansion under its new leadership.

Virtual care will take centre stage at the Digital Health Institute Summit in Melbourne next week as the COVID-19 pandemic continues to supercharge the adoption of digital health solutions throughout the healthcare system.
Digital health in practice is also a big topic as local, regional and national solutions that have been developed conceptually over many years are fast-tracked into real-life use, and new technologies to handle mass vaccination programs are rolled out in a hurry.

Queensland Health has released a 10-year digital strategy for rural and remote healthcare, promising to move the state’s healthcare system from digital ready to digital by default in the next decade.
The strategy builds on the 2016 digital health strategic vision for Queensland and its accompanying eHealth investment strategy, and envisions that all rural and remote health services across the continuum of care support highly mobile and digitally enabled workflows, with ubiquitous telehealth, virtual and integrated care.

Western Australia’s new COVID Care at Home program is using technology from Sydney’s CareMonitor to support and monitor people who have received a COVID positive test result at home.
It is also being used by St Vincent’s Hospital to deliver care to patients in the community, and by Hunter New England Local Health District to deliver hospital in the home services.
The Australian Department of Health has launched a new COVID-19 support portal on the My Aged Care provider portal as the federal minister for aged care services, Richard Colbeck, increasingly comes under fire for the crisis in the sector.
The department has set up a new helpline through Healthdirect for residential aged care facilities managing COVID-19 outbreaks, staffed 24/7 by registered nurses to provide advice on what do to if residents test positive, limiting transmission and whether residents might be candidates for oral antiviral treatments.

The New Zealand Ministry of Health is live with a suite of digital solutions to help COVID-19 positive people self-manage in the community, despite a few hiccups with the national COVID-19 clinical care module (CMMM) following the country’s move to phase 2 of managing the Omicron outbreak.
Omicron-positive patients will predominately be expected to self-manage at home, but digital solutions are being rolled out to help them as well as people who may need more support, Ministry of Health director-general Ashley Bloomfield said.

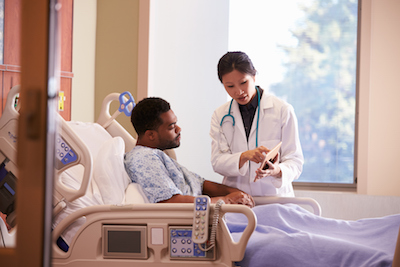
The Australian Digital Health Agency (ADHA) has released version two of its HIPS provider app, renaming it as HIPS Mobile and introducing new features such as “gain emergency access” functionality.
The technology is used by hospital clinicians to have mobile device access to patient My Health Record information at the bedside or remotely.

Dunedin’s Mercy Hospital has rolled out Rauland’s Concierge patient engagement platform in its newly opened Callaghan ward, deploying the solution on Siemens’ HiMed cockpits at the patient’s bedside.
The solution has also been deployed recently at Gold Coast University Hospital to support remote consultations in COVID-19 wards.

Medical billing specialist Synapse Medical has joined up with cloud-based medical imaging solution vendor IMEXHS to provide an integrated billing solution for medical imaging.
The agreement will see Synapse’s medical billing system integrated into IMEXHS’s Aquila product to digitise the process from patient appointment through to receipted payments.

NSW Health secretary Elizabeth Koff has been appointed as managing director Telstra Health, taking over from Mary Foley, who is retiring from full-time executive roles.
Professor Foley will join the Telstra Health board as a non-executive director and serve as a special adviser to the business.

Oracle’s plans for Cerner, FHIR endpoint progress, patient access to EHR notes, South Korea’s QR moves, wearables trialled for cancer care, EMR data mined for long COVID, patient pathways for elective surgery
Voice and NLP, global expansion key for Oracle-Cerner success
Healthcare IT News ~ Mike Miliard ~ 08/02/2022
It's a very rational acquisition considering that Cerner uses Oracle for its Millennium applications and EHR.

Telehealth and its various policy and political ramifications was back in the news this week, with the Royal Australian College of General Practitioners (RACGP) again changing its policy position on MBS funding of primary care telehealth, despite previous lobbying efforts to the contrary.
We’ve been critical of the changing position of the college on Medicare-funded telehealth and its fellow travellers at the AMA in the past, but this week we saw a triple backflip with pike as Omicron swept through the land. We have witnessed the medical fraternity going from dead set against telehealth in primary care to agreeing it is essential in a pandemic, but all of this is conditional it seems on doctors’ income not being affected.

Royal Melbourne Hospital has implemented a device interrogation service in rural Victorian pharmacies to monitor patients with implantable cardiac devices remotely to help reduce unnecessary in-person interactions during the COVID-19 pandemic.
The project is using remote device interrogation kiosks in two pharmacies to interrogate cardiac implanted electronic devices (CIED) such as pacemakers without the need for patients to travel to Melbourne.

New Zealand’s Northland District Health Board is back in the market for a replacement for its Jade community care solution, with the intention of eventually rolling out the new system to the Auckland metropolitan area.
The solution will support referral, case and bed management, prescribing, care planning, group and individual patient scheduling and clinical documentation for community care and inpatient mental health services.

South Eastern Sydney Local Health District (SESLHD) has developed a virtual health strategy to accompany the opening later this year of its new integrated acute services building at Prince of Wales Hospital (POWH).
The virtual health strategy is aimed at integrating hospital services with the community and the patient’s home to help reduce demand on the hospital, which is projected as an additional 50 acute care beds in the next five years.

The Australian government is touting $24 million in funding as a way to improve acute care systems and reduce waiting times in hospital emergency departments.
Citing figures from the Australian Institute of Health and Welfare (AIHW), the government says that despite declines during the early months of the COVID-19 pandemic, presentations to public hospital EDs in every state and territory continue to rise by an average of 3.2 per cent a year.

Queensland Health is planning an enterprise-wide roll-out of automated dispensing cabinets (ADCs) in its hospital and health services using a central ADC solution that can potentially incorporate multiple vendor solutions.
ADCs are already used in nine Queensland Health hospital and health services (HHSs), but under a new tender issued this week, the organisation says it is looking to establish a panel of one or more suppliers to provide an enterprise-wide ADC server solution, along with ADC devices, software, support, maintenance and implementation services.
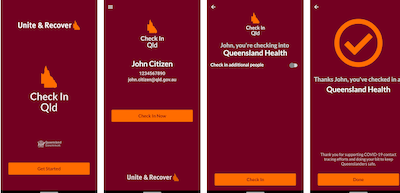
The ACT government is making changes to its widely adopted Check In CBR app to enable automatic notification of users if they have been at a higher risk setting during a COVID-19 exposure.
The move comes as both the ACT and Queensland relax rules on mandatory check ins of QR codes using the app, which was first developed by ACT Health and is also used in Tasmania and the Northern Territory.

Australian and New Zealand pharmaceutical wholesalers Symbion and ProPharma have signed long term deals to continue using ASX-listed Corum Group’s PharmX platform.
PharmX is an ordering platform used by about 6000 community pharmacies to manage supplier accounts.

Indonesia’s plans for digital health transformation, funding for India’s digital health system, adopting and implementing digital tools in large health organisations, NHS Digital merger details, tech for NHS England’s integrated care systems, migrating veterans’ data from VistA to Cerner, lobbying for telehealth extension
Ministry reveals challenges to digitize health services in Indonesia
Antara ~ Arnidhya Z, Kenzu T ~ 03/02/2022
In 2022, the Health Ministry plans to develop a big data system that is based on integrated electronic health records.

There was welcome news in the primary care sector this week with a new trial being launched in Victoria to use secure messaging technology to inform GPs if patients at medium risk of hospitalisation for COVID-19 have tested positive. The trial is using existing secure messaging technology and vendor directories for patients receiving in-home monitoring from programs like hospital in the home or HARP, and also taps into the Victorian COVID Positive pathways program.
Hopefully, the trial will go some way to solving problems for GPs in actually knowing which of their patients are positive and may need extra support. It doesn’t really solve a problem that former AMA president Mukesh Haikerwal has raised about immediately alerting GPs to ensure at-risk patients receive treatment straight away, but it’s a start at least.

MidCentral District Health Board (MDHB) has gone to market on behalf of six North Island DHBs for a smart eReferrals, intelligent scheduling and appointment booking platform.
The goal is to efficiently coordinate, communicate and integrate patient care flows, including between primary, ambulatory, allied and community care services, with a view to delivering care closer to the home and within community settings as models of care evolve over time.

Practice management software vendor Best Practice has obtained an extension for its customers to transition to the new Medicare Web Services regime, but they will still need to have the new PKI certificates installed prior to the original deadline of March 13.
Best Practice has been building its Medicare Web Services-enabled package, Saffron service pack three (SP3) for some time and had expected to have it released late last year.
It now says that while the upgrade will be released this month, it has obtained a three-month extension for users from Services Australia, with a new deadline of Sunday, June 19.

Big four consulting firm Deloitte has acquired Sydney-headquartered health technology consultancy The Checkley Group, adding to its health sector advisory practice.
The Checkley Group, founded by managing director Bruce Pedersen in 2007, is well known for its skills in areas such as electronic medical record implementation evaluations and enhancements, health technology strategy and innovation, enterprise and solution architecture and program integration.

eHealth NSW has kicked off the first phase of an outpatients referrals management solution, which has been trialled by several general practices in the NSW Northern Rivers region before being rolled out to two local health districts early this year.
eHealth NSW is working with the NSW Ministry of Health and clinicians from the LHDs to deliver the digital outpatient referral management system, which is using HealthLink’s SmartForms technology and its referral management system (RMS).

Telstra Health is providing virtual care technologies for two new Southern Adelaide Local Health Network (SALHN) services that care for older people outside of hospital.
The Complex and RestorativE (CARE) service and Geriatric Evaluation and Management (GEM@Home) are using digital health solutions from Telstra Health’s suite of virtual care technologies, including My Care Manager, Bluetooth observation devices and passive environmental monitoring.

Two primary health networks in Melbourne are helping to pilot a program in which patients assessed as medium risk of hospitalisation if contracting COVID-19 will have their GPs alerted by secure messaging.
The pilot program is being implemented by Eastern Melbourne PHN and North Western Melbourne PHN to allow consumers assessed as medium risk by Healthdirect Australia’s call agents to consent to have an outcome of their clinical risk assessment sent via secure message as a notification to their GP.

Remote patient monitoring device distributor Propell Health has won a contract with Perth’s East Metropolitan Health Service (EMHS) to provide wearable technology for patients awaiting clinical assessment in emergency departments.
The solution aims to monitor vital signs and identify changes in the patient’s condition, including early signs of patient deterioration. The technology will be rolled out at Royal Perth Hospital (RPH) and Armadale Health Service (AHS) under the HIVE (Health in a Virtual Environment) remote monitoring service.

The SA Ambulance Service (SAAS) is in the market for an electronic patient care record (ePCR) to replace its current paper-based patient cards, joining all of the other state and territory ambulance services to roll out an electronic system.
SAAS is also in the market for mobile devices such as rugged laptops and smartphones or tablets for each clinicians, allowing them to enter observation details in real time while on scene with the patient.
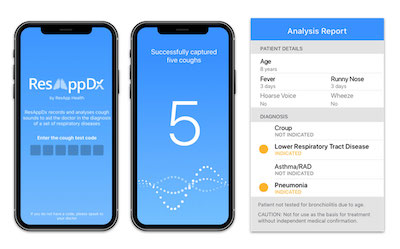
ResApp Health’s smartphone-based acute respiratory diagnostic test ResAppDx has now been implemented in Doctors on Demand’s online telehealth platform.
Doctors on Demand joins Coviu and Phenix Health in implementing the app, which uses machine learning algorithms that analyse a patient’s cough sounds to diagnose lower respiratory tract diseases such as pneumonia and asthma exacerbations.

Digital health investment bubble, Oracle’s Cerner buy dissected, HoloLens in aged care, US trusted exchange framework, IBM Watson Health carved up, mental health mobile apps don’t stack up, virtual care can reduce ED presentations
Investors disagree on whether digital health is in a bubble after another record funding haul in 2021
MedCity News ~ Arundhati Parmar ~ 20/01/2022
Everyone agreed on one thing though: valuations need to come down.

Just as telehealth dominated the last two years of digital health, remote monitoring is likely to dominate the next: that’s pretty much our prediction for the coming year or two under these strange days indeed. Everyone is getting in on the remote monitoring act and it makes sense, clinically, practically and financially.
We reckon the alleged revolution in telehealth in Australia has turned out to be overhyped in a practical sense. While the acute care sector has struggled valiantly over the years to develop funded telehealth models of care using video conferencing, the modality has not been taken up in primary care in the slightest, predominantly due to funding concerns. But when funding does comes through – such as, say, temporary MBS items during a pandemic – phone calls are not really what telehealth is all about. GPs claiming for monitoring known patients by phone should be a given under a properly funded primary care system. Unfortunately, we are stuck with fee for service so even the most minor funding shift is heralded as revolutionary.

Residential aged care managed services provider Third Age Health is rolling out Celo’s collaboration tool to its clinicians to prepare for the expected widespread Omicron outbreak in New Zealand.
Third Age Health provides care for roster rounds, on call and after hours to more than 50 residential aged care facilities. It also owns several general practices.

Queensland’s Mater Health has rolled out Philips’ QuestManager virtual monitoring technology to look after COVID-19 patients in their own homes.
The technology was launched just after Christmas and is caring for more than 130 patients on Mater’s virtual ward, but is capable of supporting tens of thousands of people if required.

St John of God Health Care will hold a preliminary trial of Citadel Health’s Charm Evolution oncology information management system at its Comprehensive Cancer Centre at St John of God Subiaco Hospital later this year.
The system will be the hospital’s first centralised oncology patient record combining treatment plans, appointment scheduling and simplified reporting.

Practice efficiency and appointment booking system vendor AutoMed Systems has released a new debtor management utility that automates tasks such as the issuing of invoices and collection of payment for services like telehealth consults to its utility suite.
It follows the release late last year of an appointment book audit utility in AutoMed’s dashboard aimed at automating routine administrative tasks and freeing up practice management and reception staff, including consent forms, appointment bookings, maximising added value clinics and improve practice data quality for PIP QI purposes.

ASX-listed patient engagement firm 1st Group plans to acquire telehealth technology vendor Visionflex in a merger aimed at offering an end to end clinical telehealth service to the local market.
Visionflex markets a range of solutions including all-in-one telehealth solution called ProEX that includes video conferencing as well as clinical devices and cameras for remote diagnosis and monitoring, while 1st Group markets the MyHealth1st online appointment booking system for general practice, allied health, pharmacy and dental providers, amongst other offerings.

St Vincent’s Alcohol and Drug Service is live with its clinical advice line telephone service to support the roll out of the SafeScript NSW real-time prescription monitoring (RTPM) system.
The first phase of SafeScript NSW rolled out in the Hunter New England and Central Coast regions last November, with the other parts of the state due to come on line in the next six months.

Western Sydney Primary Health Network (WentWest) has appointed Paul Nicolarakis as its inaugural chief data officer.
Dr Nicolarakis, a qualified medical doctor, will focus on developing and implementing a new information strategy covering data governance and infrastructure.

Telehealth platform Coviu has partnered with Propell Health, the Australian and New Zealand distributor of iHealth devices, to offer an integrated telehealth and remote patient monitoring (RPM) solution for the management of COVID-19 patients.
The solution is aimed at GPs and practice nurses to allow them to remotely monitor patients during virtual consultations using the hospital-at-home care model.
Welcome back to another thrilling year in the world of digital health, which kicked off for the new year just as we ended the old: consumed by confusion over telehealth policy. The Australian government seems to change the rules on telehealth as often as it changes its underwear and it must be said, the elastic is getting a little bit frayed.
Last Sunday, after repeated claims about telehealth being “permanent” and “10 years rolled out in 10 days”, we experienced yet another change in the rules. According to various statements from the Department of Health, health minister Greg Hunt, the AMA and the RACGP, the rules that applied to MBS-funded telehealth in the early stages of the pandemic were to be reinstated for the next six months to help general practice cope in the face of the Omicron wave.

Digital health regulation, voice recognition in healthcare, Singapore’s TraceTogether, Zoom’s view on digital health, virtual EDs in Toronto, Doctor Anywhere in SE Asia, unique health identifiers, IBM’s troubles offloading Watson Health, Stryker buys Vocera, Oracle buys Cerner
Apple (and everyone) needs harmonized digital health regulation
Computerworld ~ Jonny Evans ~ 21/01/2022
Perhaps Apple's hopes to innovate in digital health have been held back by the lack of an internationally agreed upon set of standards.
Why voice recognition is the new competitive battleground in healthcare's digital transformation
Healthcare IT News ~ Paddy Padmanabhan ~ 20/01/2022
As ambient technologies improve, additional use cases to leverage voice will emerge – that leaves us with the question of how patients and physicians are responding to voice-enabled tools in their healthcare encounters.
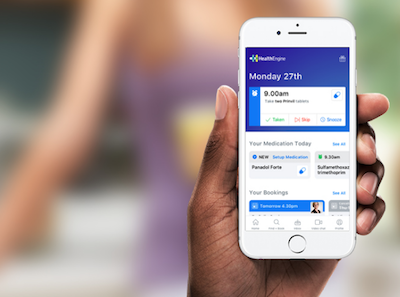
Online appointment booking and directory service HealthEngine has bought medical practice digital health solutions provider Healthsite, with plans to offer healthcare practices more access to software and marketing solutions.
A Healthengine spokesperson said that with the acquisition, Healthsite will become a subsidiary of Healthengine but will continue to operate with its own leadership team.
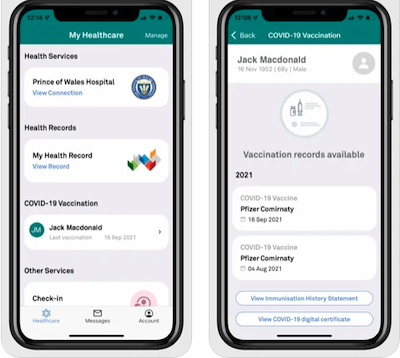
Telstra Health has upgraded its HealthNow mobile app to enable users to access and share their COVID-19 digital certificate.
HealthNow is one of two apps in Australia that enables secure access to a user’s My Health Record, which contains Australian Immunisation Register data as well as COVID test results and access to the digital certificate.
Private equity fund-owned Citadel Group has finalised the purchase of market-leading medical software vendor Genie Solutions, and is already working on ways to link Genie’s private specialists to Citadel’s wider footprint in diagnostic software.
The Citadel Group, owned by private equity firm Pacific Equity Partners, announced it would buy Genie Solutions last year. While the price was not disclosed, it is understood to have been in or around $260 million.

A pop-up Head to Health service in the ACT designed to help Canberrans struggling with mental health issues during the COVID-19 pandemic is using CareMonitor’s care coordination, remote patient monitoring and telehealth platform to deliver mental health services.
The Canberra Head to Health Centre is one of the first in a network of community mental health centres being rolled out, providing help for people experiencing high levels of distress, or who are at heightened risk of suicide.

Hills Health Solutions has teamed up with Melbourne firm Olinqua to offer a converged IP-based platform that brings together nurse call and critical messaging for hospitals and aged care facilities.
The solution has already been deployed at Melbourne’s Austin Hospital and Canberra Hospital, and is aimed particularly at medical emergency situations.

The Western Australian government has awarded a $39.6 million contract to the joint venture between Calvary Health Care and Medibank to operate a virtual care home monitoring service for people in home quarantine.
The service will carry out triage and regular remote video or telephone call monitoring of patients as WA gears up for a relaxation of COVID border restrictions on February 5. The procurement was a limited tender under emergency rules.

Two Australian primary health networks (PHNs) are using Healthily’s GoShare Plus to create and share targeted COVID-19 communications for Aboriginal and Torres Strait Islander communities and culturally and linguistically diverse (CALD) people to encourage vaccination and testing.
The interactive digital health packages include a video message from key community leaders speaking about the importance of vaccinations and how COVID-safe behaviours can help protect people.
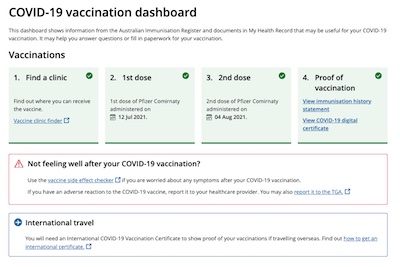
The Australian Digital Health Agency (ADHA) has added a new COVID-19 dashboard to the My Health Record system, allowing users to see all COVID-19-related information in one place.
This includes records of vaccination details, test results, medical conditions, relevant medicines and allergy information along with links to Healthdirect’s COVID-19 vaccine clinic finder and side effect checker from within the dashboard.

NAB’s HICAPS healthcare claims subsidiary has entered into a sale and purchase agreement with technology developer InLoop to acquire Lantern Claims, which operates health claiming platform LanternPay.
NAB plans to integrate HICAPS with LanternPay to provide a digital platform with real-time approvals and faster payments for healthcare providers.

The Australian government has agreed to restore access to MBS-funded telehealth using the same arrangements introduced early in the Covid-19 pandemic.
The measures, which will last for six months, will allow GPs to bill for telehealth Level C consultations and allow private telehealth providers to conduct relevant consultations with patients by phone or video.
Pulse+IT has been running our annual eHealth year in review series this week as we wind down for an extended holiday, but we did take a bit of time out to read up on Australian health minister Greg Hunt’s announcement that telehealth will apparently become a “permanent” feature of the MBS. In amongst a lot of hyperbolic announcements amounting to what seems like eleventy billion dollars in funding for the government’s COVID-19 response, we discovered that the “permanent” telehealth measure merely amounted to just over $100 million over four years.
It appears that the guts of this measure is that a patient can be phoned or consulted by video and the GP can claim for it if they have seen that patient in person in the previous 12 months, as is allowed now under the COVID-19 provisions. The only change is the permanent bit. However, the government’s plans for voluntary patient registration are destined to restrict this further in the future to only those patients registered with one practice. It’s not exactly the free for all the press releases promise but Mr Hunt managed to roll out RACGP president Karen Price for the announcement, which is apparently all that matters.

Pulse+IT publisher Simon James’ story on NSW Health’s “broken” vaccination booking system was the most popular article for the year by a country mile. Six of the top 20 most-read stories were about the various booking systems rolled out, including HealthEngine winning the contract for a national solution, ACT Health’s MyDHR solution and its feat in going live with its Epic EMR for phase 1 vaccinations were also of interest.
Telstra Health’s acquisitions of MedicalDirector and PowerHealth Solutions, its new health exchange from TELUS and its Kyra platform all made the top 20, as did our interview with Dedalus Asia Pacific managing director Darryl Goodall about its post-DXC strategy.
Copyright © 2025 Pulse IT Communications Pty Ltd. No content published on this website can be reproduced by any person for any reason without the prior written permission of the publisher. If your organisation is featured in a Pulse+IT article you can purchase the permission to reproduce the article here.
Website Design by Get Leads AU.