Healthcare clinics across New Zealand and Australia are being offered the ability to build their own virtual services using TytoCare’s complete virtual clinic solution – featuring a specialised digital medical examination device and online portal.
The TytoCare device is a handheld, AI-enabled remote examination tool that allows patients and healthcare assistants to capture clinical-grade readings – from heart and lung sounds to throat and ear images – which can then be reviewed by clinicians virtually through the TytoCare platform.
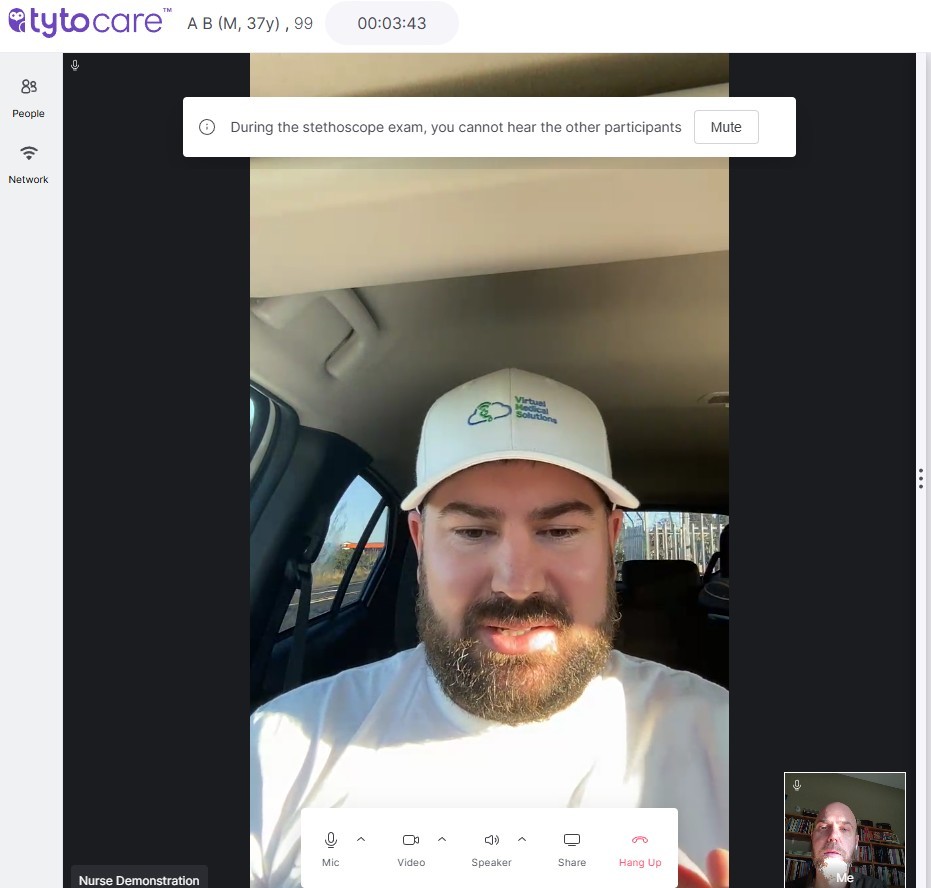
The platform includes an online clinician portal and app, with video consultation capabilities for clinicians and patients to interact while using the remote device.
TytoCare’s New Zealand distributor, Virtual Medical Solutions (VMS) director and co-founder Adam Benko told Pulse+IT he aimed to help New Zealand clinics to deliver remote healthcare “their own way,” empowering them to build, run and staff their own virtual services.

TytoCare is currently being used in several remote locations across New Zealand and Mr Benko conducted a live demonstration with perfect results for Pulse+IT from his car parked remotely on the side of the road near National Park, using the TytoCare video platform over mobile data.
He said the government’s recent health funding announcement, aimed at boosting 24/7 virtual and urgent care services, presented opportunities for investment in health tech such as TytoCare, and could “create more access to primary healthcare services for patients while also maximising the reach of the existing primary healthcare workforce.”
“Our goal is to enable healthcare providers to build their own virtual service, so that they’re not having to outsource it,” Mr Benko said.
“They can control it. Any clinic in New Zealand can now have a really solid platform, be able to service their own registered patients and manage their own staffing.
“It’s about employing your own workforce, building that extension of your clinic, and having a service that gives you continuity and sustainability.”
AI FEATURES
Mr Benko said a key feature of the device was its real-time AI guidance, which ensured recordings met clinical quality standards, while “also making the user experience really simple so that anyone can use it.”
“In the throat exam, if I was to use the device on myself, when I point it at my throat, I get a green tick. That’s the AI looking,” Mr Benko said.
“If I press too hard with the stethoscope attachment, it flashes up ‘reduce pressure’. If there’s background noise, it tells me ‘noise interference’ and it won’t let me send that recording until it’s clean. The device is working to ensure what’s going through is usable.”
REMOTE USE
Mr Benko said that with the ability to be deployed anywhere – from pharmacies and GP clinics to marae and even camper vans-turned-mobile clinics – VMS was currently targeting rural and remote access gaps, but also saw opportunities in urban, time-poor communities.
“There are lots of opportunities to improve access to primary healthcare. We’ve got a campervan up in Northland kitted out into a mobile clinic that connects back to a doctor sitting in town.
“This could be used on Great Barrier Island, Stewart Island, even the Chathams or Niue – places where people are currently flown to the mainland for care. Using TytoCare would be much more efficient.”
“The obvious user case is within rural communities, but urban would work just as well – busy working parents who are having to take time out their working day to get an appointment with their healthcare provider, or for their kids, taking them out of school – you could have an after hours service that uses this, where you can access it from the comfort of your home. That’s the future of healthcare and this is here now, ready to make a difference.”
Mr Benko said that while TytoCare is relatively new to the New Zealand market, it has been available internationally for over nine years and is currently used in 32 countries.
“One provider in Israel has over 70,000 units out in the community. Each home device can serve up to 10 patients. That’s a potential reach of 700,000 people for one provider,” Mr Benko said.
“What they’re offering is a blend of virtual and in-person. Virtual doesn’t solve everything – but when it can help avoid an unnecessary ED trip or after-hours urgent care visit, that’s a huge benefit.”
DATA PRIVACY AND AI USE
TytoCare uses AWS cloud hosting based in Sydney, and adheres to HIPAA, GDPR and NHS-level data privacy standards. Mr Benko said only minimal patient data was required and anonymous profiles were also possible.
“We don’t need the patient’s name. You can literally set someone up as ‘Adult Male Patient’. All that’s needed is a rough date of birth and sex – because some features change depending on if the patient is a child or adult.”
None of the video or exam data is stored unless the “record” button is pressed. When it is recorded and uploaded, it is stored anonymously and encrypted.
“Those recordings help train the AI. Last year, TytoCare released a wheeze and crackle detection feature for lung exams that’s the AI listening and flagging abnormalities for the clinician to check. That’s the future of TytoCare.”
That particular AI feature is FDA-approved and used in the US but not yet available in Australasia, but Mr Benko said “once we get more volume here, there’ll be more incentive to bring those features over.”
INTEROPERABILITY AND INTEGRATIONS
TytoCare has APIs available for integration with PMS and EMR systems, but Mr Benko said that in practice, most clinicians currently use it alongside their existing systems.
“Doctors have their PMS open on one screen, TytoCare on the other. All referrals and prescribing tasks are completed through the PMS as if the patient was in the room,” he said.
“And now, with AI notetaking tools like Heidi, some doctors are running everything in parallel – they just talk to the patient, and the notes go straight into the PMS. It’s really efficient.”
FUTURE PLANS
Mr Benko said he was currently looking at how to make TytoCare even more accessible, “whether that means working with the iwi to place a device in a marae, or in a satellite clinic where it’s easier for whānau to get to.”
“The value is obvious, the need is obvious. Now it’s about making people aware this exists – and helping them use it in a way that works for their community.”
TytoCare devices are also TGA approved in Australia, with use cases including Northern Health in Victoria – which was the first public health service in Australia to launch the device.





